Hey everyone! Many members tend to have a check list or sort of guideline they follow when giving a radio or a transfer of care report to the hospital. I'm afraid of arriving at the hospital and then clamming up in front of the doctor because I panicked and don't know what to say. Can someone please suggest to me any mnemonics, lists, or guidelines to help me remember what I should and shouldn't say on either of these reports? Many thanks in advance
Navigation
Install the app
How to install the app on iOS
Follow along with the video below to see how to install our site as a web app on your home screen.
Note: This feature may not be available in some browsers.
More options
Style variation
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Radio and TOC reports
- Thread starter ReeNadeau
- Start date
DrParasite
The fire extinguisher is not just for show
- 6,380
- 2,240
- 113
truth be told, it depends on the agency and depends on the hospital. I used to work where we transported to two hospitals in city; at one hospital, when we called in a radio report it went to their dispatch center, and rarely was relayed to the ER (because, quite honestly, the ER didn't care). The exception to this was if we had a sick patient, then ALS was speaking to their medical control, who were ER attendings in that ER. The other exception was if we were a BLS crew, and needed intervention on arrival; then the message would be relayed.
We spoke to a nurse in the ER at the other hospital, so the reports were a little better as the radio reports are primarily designed to give the ER that a patient was coming to the ER. rarely were anything more than basic details given (age, chief complaint, interventions given, resources needed on arrival) were pretty much it. the TOC was in person, face to face, and provided a much better story.
We spoke to a nurse in the ER at the other hospital, so the reports were a little better as the radio reports are primarily designed to give the ER that a patient was coming to the ER. rarely were anything more than basic details given (age, chief complaint, interventions given, resources needed on arrival) were pretty much it. the TOC was in person, face to face, and provided a much better story.
EpiEMS
Forum Deputy Chief
- 3,845
- 1,166
- 113
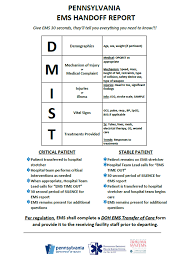
MIST is an easy one - see https://www.crisis-medicine.com/mist-report-a-simple-way-to-convey-information/ for example.
Here’s a straightforward one for transfer of care in person:
Mechanism/medical complaint - This is Mrs. Jones. She’s a 68 year old female who experienced a mechanical fall and is complaining of 6/10 right hip pain. No head strike, no LOC, no anticoagulants, no allergies, meds are ASA and a multivitamin daily.
Injuries/illness - The right leg is externally rotated and shortened. Bruising on right hip. Pulse, motor strength, and sensation intact. No other injuries noted.
Signs (vital signs)- P 90, BP 130/90, SpO2 98%, BGL 100, temp 99 F
Treatments - pillows, bound injured leg to uninsured leg for stabilization & applied ice for pain management
Same thing for radio:
Good afternoon, this is A100, BLS unit, 10 minutes out from your facility, inbound with a 68 y/o female with suspected right hip fracture from a mechanical fall on same level. No anticoagulants, no head strike, no LOC. Patient is resting comfortably, vitals are within normal limits. No significant interventions being provided. Any questions?
Here’s a straightforward one for transfer of care in person:
Mechanism/medical complaint - This is Mrs. Jones. She’s a 68 year old female who experienced a mechanical fall and is complaining of 6/10 right hip pain. No head strike, no LOC, no anticoagulants, no allergies, meds are ASA and a multivitamin daily.
Injuries/illness - The right leg is externally rotated and shortened. Bruising on right hip. Pulse, motor strength, and sensation intact. No other injuries noted.
Signs (vital signs)- P 90, BP 130/90, SpO2 98%, BGL 100, temp 99 F
Treatments - pillows, bound injured leg to uninsured leg for stabilization & applied ice for pain management
Same thing for radio:
Good afternoon, this is A100, BLS unit, 10 minutes out from your facility, inbound with a 68 y/o female with suspected right hip fracture from a mechanical fall on same level. No anticoagulants, no head strike, no LOC. Patient is resting comfortably, vitals are within normal limits. No significant interventions being provided. Any questions?
CCCSD
Forum Deputy Chief
- 2,036
- 1,299
- 113
Memorize your PCR.
Report in that format.
Always the same each time.
Report in that format.
Always the same each time.
NomadicMedic
I know a guy who knows a guy.
- 12,246
- 7,028
- 113
DMIST is what we use.
planetmike
Forum Lieutenant
- 203
- 61
- 28
Someone asked a similar question a couple days ago over on Reddit. Here is my response:
I'm the guy at our Level 1 trauma center taking the report. We use phone for reports. Keep it short and relevant. Identify your truck (jurisdiction and number). Type of Alert (Trauma, Stroke, Heart, OB) if any. Patient age and male/female. Chief complaint. Interventions. Vital signs. Covid pre-screen status. Where are they coming from if it's a nursing home or physician office. How long until you arrive.
If it is going to be an Alert of some type, start off with that so we can get the appropriate physician in to hear your report.
We do not need race, social security number, medications they take, allergies, or other history.
Don't just hang up at the end of your report. We might have questions we have to ask. For us, a stroke or heart alert we have to get specific additional info for the on-call medical specialty team.
Don't speak too quickly or softly. Enunciate, especially if you're wearing a N95 with the sirens going.
When giving numbers, repeat them after giving the entire number (120/80, one two zero over eight zero).
Know what your hospital's Alerts are, and what criteria trigger those alerts. At our trauma center, A "Gold" Alert is a more serious "Trauma" Alert. Both have criteria (vital signs, gcs, specific injuries) that local EMS providers should know. You should learn what your local hospitals’ criteria are for your alerts. They will be very specific to your systems.
Like every skill, you get better by doing it.
I'm the guy at our Level 1 trauma center taking the report. We use phone for reports. Keep it short and relevant. Identify your truck (jurisdiction and number). Type of Alert (Trauma, Stroke, Heart, OB) if any. Patient age and male/female. Chief complaint. Interventions. Vital signs. Covid pre-screen status. Where are they coming from if it's a nursing home or physician office. How long until you arrive.
If it is going to be an Alert of some type, start off with that so we can get the appropriate physician in to hear your report.
We do not need race, social security number, medications they take, allergies, or other history.
Don't just hang up at the end of your report. We might have questions we have to ask. For us, a stroke or heart alert we have to get specific additional info for the on-call medical specialty team.
Don't speak too quickly or softly. Enunciate, especially if you're wearing a N95 with the sirens going.
When giving numbers, repeat them after giving the entire number (120/80, one two zero over eight zero).
Know what your hospital's Alerts are, and what criteria trigger those alerts. At our trauma center, A "Gold" Alert is a more serious "Trauma" Alert. Both have criteria (vital signs, gcs, specific injuries) that local EMS providers should know. You should learn what your local hospitals’ criteria are for your alerts. They will be very specific to your systems.
Like every skill, you get better by doing it.
- 7,904
- 2,879
- 113
Was going to add the D or I (identify) to @EpiEMS 's post. Identification is important and also makes your patient feel better.
Come up with your own basic report, and give it: unless you only transport to a 1 or 2 major hospitals don't worry about the color coded alerts: (unless all the hospitals use the same alert systems) because in a lot of cases different hospitals used different alert codes: just to be annoying to us.
This is what I do: This is John on Unit ##: ___ minutes out; I have a {Trauma, STEMI, Stroke, etc) 65 y/o F, mech of injury/illness, VS (if important {HTN, hypotensive, HR up or down etc}); important info for the alert (stroke, last time seen normal for example). Do you require anything further?. 9 times out of 10 if it isn't an alert that I called in, when we get to the hospital and a room, none of my report that I called in gets to the nurse in the room so it doesn't matter much. But heaven help me if we don't call 1st.
Charge nurses still manage to screw up reports when you call them in, I have been yelled at for not transporting to closer hospitals with a critical patient, (when they were the closest hospital) that 1 yelled at me so much when we arrived, that the ED doctor made security escort her to the break room or not flying them during a blizzard when no helicopter for 200 miles could get off the ground, although the weather was great where we started.
Remember whatever you give as a report, a partner or a nurse won't like it and will tell you it is wrong. Don't worry about it. I have been doing this for 25 years, and it is fun to be told by someone who has given 5 phone reports that mine isn't very good
This is what I do: This is John on Unit ##: ___ minutes out; I have a {Trauma, STEMI, Stroke, etc) 65 y/o F, mech of injury/illness, VS (if important {HTN, hypotensive, HR up or down etc}); important info for the alert (stroke, last time seen normal for example). Do you require anything further?. 9 times out of 10 if it isn't an alert that I called in, when we get to the hospital and a room, none of my report that I called in gets to the nurse in the room so it doesn't matter much. But heaven help me if we don't call 1st.
Charge nurses still manage to screw up reports when you call them in, I have been yelled at for not transporting to closer hospitals with a critical patient, (when they were the closest hospital) that 1 yelled at me so much when we arrived, that the ED doctor made security escort her to the break room or not flying them during a blizzard when no helicopter for 200 miles could get off the ground, although the weather was great where we started.
Remember whatever you give as a report, a partner or a nurse won't like it and will tell you it is wrong. Don't worry about it. I have been doing this for 25 years, and it is fun to be told by someone who has given 5 phone reports that mine isn't very good
Fastfrankie19151
Forum Crew Member
- 43
- 6
- 8
We used dmist also and of course any other pertinent information you feel needs to be relayed but be sure to speak clearly and be sure to say any questions so they have time to ask them also don’t forget stuff like bariatric bed on standby or stuff that may be overlooked.
- 5,047
- 1,465
- 113
I've been on both sides of that radio. I'm an ED RN and generally speaking, I don't care all that much about the format you use, as long as it allows you to present the patient in a coherent manner. What I'm primarily looking for is what your ETA is and your patient's chief complaint. After that, give me a 15-20 second summary what you've found, give me some vital signs (or a reason why you haven't gotten any), and then what you've done for the patient and perhaps your plan if you're still working on things.
Now if your system mandates a specific format for certain types of patients, learn that format and use it.
One small pet-peeve of mine is when the medic's radio is turned back to dispatch immediately after giving report and not really allowing me time to ask a clarifying question. Usually it's that I need something repeated, but when I ask and there's nothing there... it's kind of (slightly) irritating. If you're asking for orders, well then you'll be looking for those orders so you'll keep your radio on until you know that I've given them or not.
I have modified the below quote to reflect how I'd generally give a radio report.
If you learn to do good radio reports and even hand-off reports to the ED, the people receiving your patient might not realize you're "only" BLS. That comes from practice, experience, and (most importantly) doing a very good assessment.
Now if your system mandates a specific format for certain types of patients, learn that format and use it.
One small pet-peeve of mine is when the medic's radio is turned back to dispatch immediately after giving report and not really allowing me time to ask a clarifying question. Usually it's that I need something repeated, but when I ask and there's nothing there... it's kind of (slightly) irritating. If you're asking for orders, well then you'll be looking for those orders so you'll keep your radio on until you know that I've given them or not.
I have modified the below quote to reflect how I'd generally give a radio report.
Where I'm at, most of the ambulances bringing patients to the ED are ALS, so when we say "ALS" instead of "BLS" we're basically saying that the patient needed some kind of ALS intervention or monitoring specifically. Our crews usually only run Code 3 for traumas that are circling the drain, someone on BiPAP or needing the BVM (or other unstable airway problem), a stroke alert, or a code that they need to transport.Good afternoon, this is A100, inbound code 2 BLS,10 minutes out from your facility, with a 68 y/o female with suspected right hip fracture from a mechanical fall on same level. Right leg is shortened & externally rotated. Good distal CSM. No LOC, no head strike, no thinners. Patient is resting comfortably, vitals are - P 90, BP 130/90, SpO2 98%, BGL 100, temp 99 F. No significant interventions being provided. Any questions?
If you learn to do good radio reports and even hand-off reports to the ED, the people receiving your patient might not realize you're "only" BLS. That comes from practice, experience, and (most importantly) doing a very good assessment.
