Part of the issue with paramedics being unable to intubate on the first time if they don't do it enough. the studies, particularly out west, support that thinking. If you have a medic who hasn't intubated a live person in over a year, can you really fault them for not being proficient in it?
This was also the area that you will have 6 to 8 paramedics on the scene of an arrest (3 on the engine, 2 on the ambulance, maybe a supervisor or a second truck), so 6 paramedics, 1 tube, you see the issue.
Compare that to my days back in NJ, where paramedics would tube 1 patient every 2 weeks (and some people it was 2 patient's a week on a bad week)... every cardiac arrest was intubated, and many were intubated in the awkward position with paramedics getting on some super sketchy floors.. 1 patient, 2 paramedics, who only handled ALS patients..... see the difference?
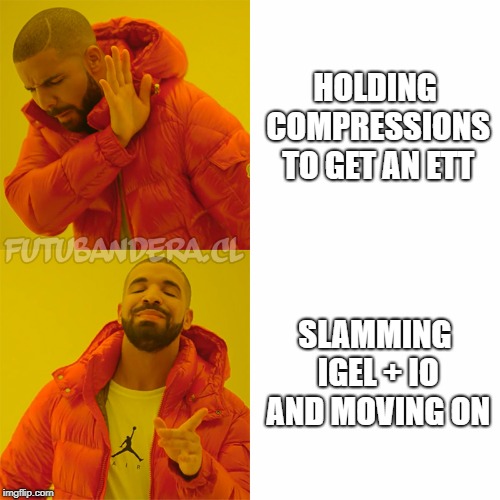
If you are going to remove ETI, and use SGA as the first line or airway management, how proficient will your crews be when they get a bad airway burn who needs an ETI ASAP, or a patient where the SGA isn't working well enough, or pick another person who needs an ETI vs a SGA? Remember, if you don't use a skill, you do lose it, as the studies have shown.