Yes, the tracings are different.
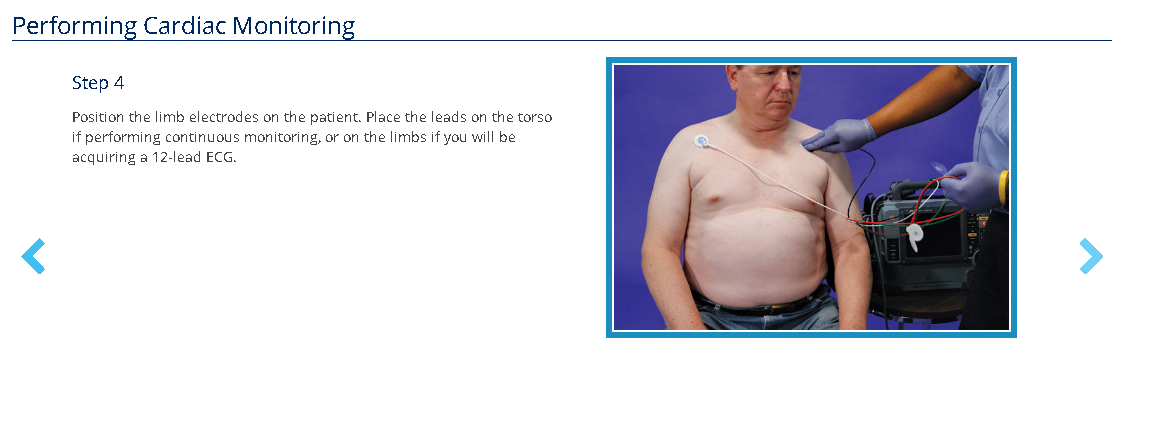
We usually start off with the bottom picture where it says step 4. We can put three to four wires "leads" on the patient, and we usually use these three to four leads to monitor the patient continuously. It might be documented as "cardiac monitoring", "3 lead ECG", or "4 lead ECG" depending on the number of wires used. We use the word "lead" interchangeably with the name of the actual wire (each wire is called a lead) and also each view of the heart the wire allows us to see, so even though there might be only 4 physical leads on the patient, it might produce 6 views/leads that we sometimes call "a quick 6".
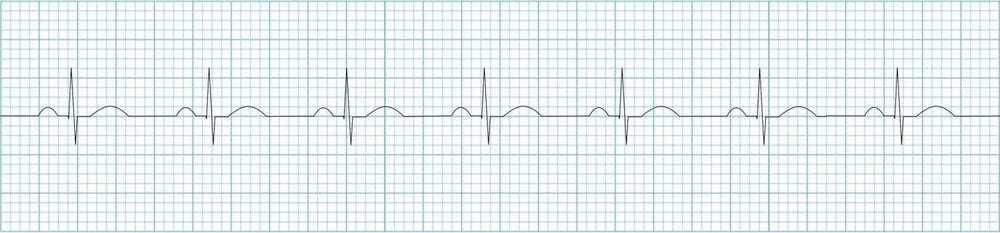
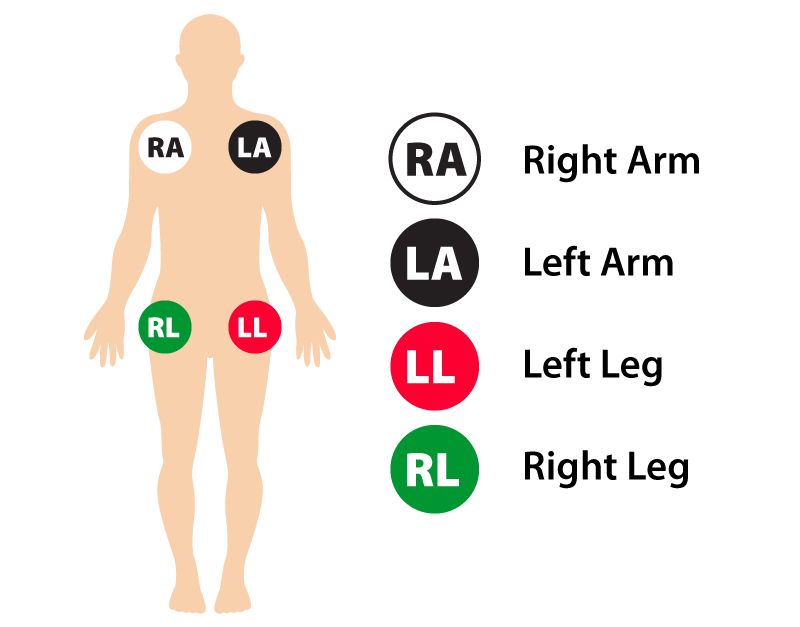
If 3 physical leads are used only, usually with the monitor called a Philips MRx, then you'd put a red (left leg (LL)), white (right arm (RA)), and black lead (left arm (LA)) on the patient to monitor them. This would produce electrical views of the heart that we would call lead I, II, and III (those are roman numeral 1, 2, and 3, so we'd literally say lead "one", lead "two", and lead "three"). In the majority of places and training, lead II is used. Lead II is observed via the right arm white lead being considered a negative point, the red foot or red left leg lead being considered the positive point, and the black left arm lead being considered the ground lead that doesn't see or do anything or than be the ground. These negative and positive points would be in comparison to the overall average/mean electrical activity of the heart.
Philips MRx
Philips 3 leads
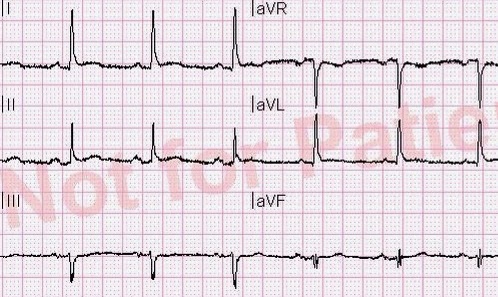
ECG Strip, usually lead II unless said otherwise
Other monitors like the Lifepak usually come with four physical wires, the same as Philips, but with a green right leg (RL) ground lead. To view lead II, you would only need to put the right arm white lead on (the negative point), the left leg/foot red lead (the positive point), and the green ground lead, which, would only show lead II, and no other lead could be seen. If you put all four wires/leads on the patient, it would produce a quick 6. With all four physical leads/wire on, you could see six leads/view lead I, II, III, aVR, aVL, and aVF.
Lifepak 15
Lifepak 4 leads
Limb leads location on patients. Philips usually has green left leg lead attached to it's "12-lead" cables, but goes in the same location and serves the same purpose by being the ground lead
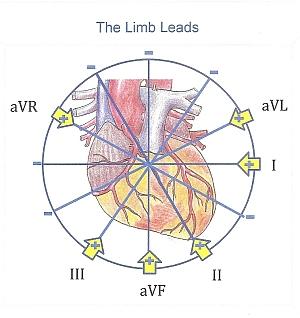
These four wires, that we call the limb leads, show us the frontal/vertical view of the heart.
Frontal view of the heart
Quick six: I, II, III, aVR, aVL, and aVF
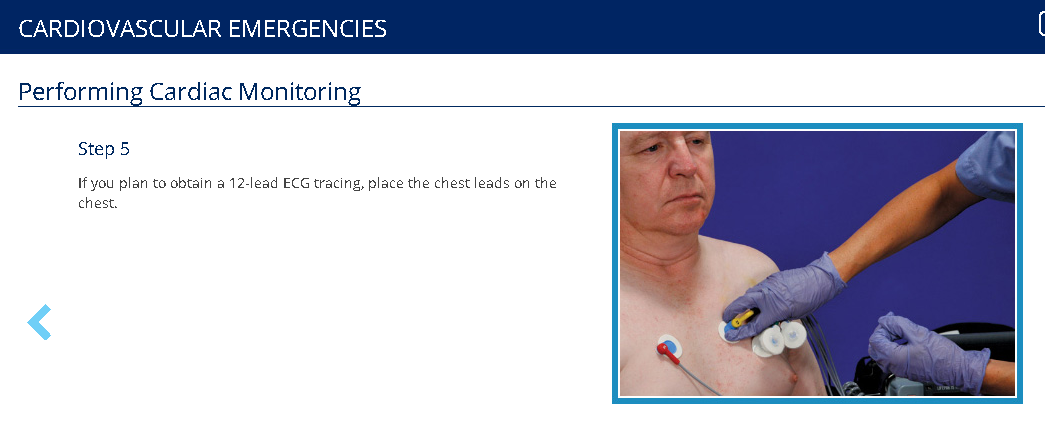
This only shows us half the picture. So what we do to get a full view of the picture is put the precordial chest leads on the patient (step 5 in the initial post).
- V1 is placed on the right side of the chest, 4th intercostal space, parasternal.
- V2 is placed on the left side of the chest, 4th intercostal space, parasternal.
- V3 is placed literally between lead V2 and V4. Usually people skip to lead V4 before placing lead V3 on.
- V4 is placed on the left side of the chest, 5th intercostal, midclavicular.
- V5 is placed on the left side of the chest, 5th intercostal, anterior axillary.
- V6 is placed on the left side of the chest, 6th intercostal, midaxillary.
Precordial chest leads
Precordial chest leads with the green right leg ground lead used on Philips MRx
These precordial chest leads give you a tranverse/horizontal view (as opposed to the frontal/vertical view of the limb leads).
Tranversed/horizontal view of the heart
12 lead: Lead I, II, III, aVR, aVL, aVF, V1, V2, V3, V4, V5, and V6
To monitor in these leads would be a little bit more work because I believe you need to have the limb leads on for them to work as well; These leads I believe use the very center of the limb leads as a second point to create a vector. The second point is called central terminus I believe. As you can see, it is kind of a pain to point on all these extra wires just to "monitor" the patient. That's why they aren't frequently used to monitor the patient, but just to get a full view of the heart. Sometimes people do like to use lead V1 to monitor for atrial arrhythmias because lead V1 rest right over the right atrium, and this could help you find something like "atrial flutter" which is a type of cardiac arrhythmia.
As paramedics, we generally do 3 leads or 4 leads to monitor the patient. When we suspect that there is an arrhythmia, ischemia "heart attack", electrolyte problem, we might do a 12-lead (limb leads and chest leads combine) to get the full view. Each lead serves different purposes that can help us identify cardiac arrhythmia (eg lead II, III, aVF, and V1 are useful in atrial tachycardia and flutter), localizing where there is heart damage in a heart attack (II, III, aVF are the inferior/bottom part of the heart. I, aVL, V5, and V6 are the left lateral part of the heart. V3 and V4 are the anterior/front part of the heart, or we can tell when there is damage to the back of the heart using the anterior part as a mirror.), or if there are electrolyte problems (particularly hyperkalemia/high potassium with tall T waves, usually I see it best in the precordial chest leads).
I would've kept this short and simple, but I feel like paramedic school usually lacks in this as well, or at least mine did. You will learn some or most of this in paramedic school, but I think it can be useful to know as an EMT working on an advance life (ALS) support unit with a paramedic why certain things may be done or why we might say something like "3 lead" vs "4 lead" or why the paramedic might not put all the wires on (my EMT will get critiqued by paramedics when she only puts the white, red, and green lead on, and they'll be like "You need to put on all of it on to work", which you actually don't). It might understand how a quick 6 might be useful, but also its disadvantage (you will miss anterior and posterior wall MIs "heart attacks" if you do not do a full 12-lead, but useful if you're afraid to give nitroglycerin to an inferior wall MI since a quick 6 does show the inferior leads "quickly").
Sorry for the novels. None of these pictures belong to me; I just stole them from Google.