TXmed
Forum Captain
- 309
- 132
- 43
So ive been told dopamine does not work in septic shock (although ive seen it in other peoples protocols). I was wanting to know the patho as to why it doesnt work. As well as why levophed does work .
Follow along with the video below to see how to install our site as a web app on your home screen.
Note: This feature may not be available in some browsers.
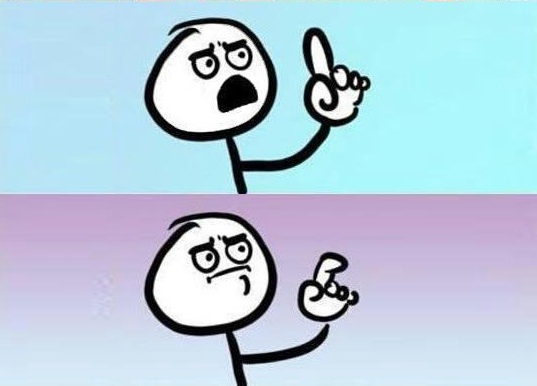
Ok. But why does dopamine NOT work ?
A Few Points on Meds:
- Dopamine has both alpha and beta (inotropic & chronotropic) properties. So it squeezes vessels, increases heart contractility and HR
- Levophed and Neo are more beta (inotropic)
- Dopamine is not good for volume-related hypotension (remember, squeezing dry pipes = no good)
Seems like some have already hit this on the head... Why is the pressure low=osmotic shift, rate / contraction increase ( chrono/ino) will capitate the pump ( can't force through or oncrease thtough rate volume that's not present) marked increased HR (chrono )in septic shock accelerates potassium dump and cardiac arrhythmia potentials... If there was no option... Bolus, Bolus, piggy Dope@ bare minimum and prepare to override pace since u won't be able to turn back... Better plan would be Neo!! or # 2 in my book high volume low dose Epi drip while watching those "T" waves w bicarbonate and cal chlor on hand...
