So just another one of my typical Call reviews / scenarios type of thing.
60yo M, A&0X4 GCS15 called for shortness of breath. Pt seems almost like a drug induced sort of Presentation, Rolling around on the bed really just "playing it up" but am on the fence weather he's just in SEVERE distress or playing it up. Very agressive and non-compliant with assessment questions, Overall home enviornment and family members suport this suspicon as well.
initial vital signs are unable to be obtained due to pt LITERALLY constantly moving and rolling around and yelling.
We get him on a tarp and carry out, and He goes limp and GCS3 with agonal respirations like 10 seconds before getting him onto the gurney.
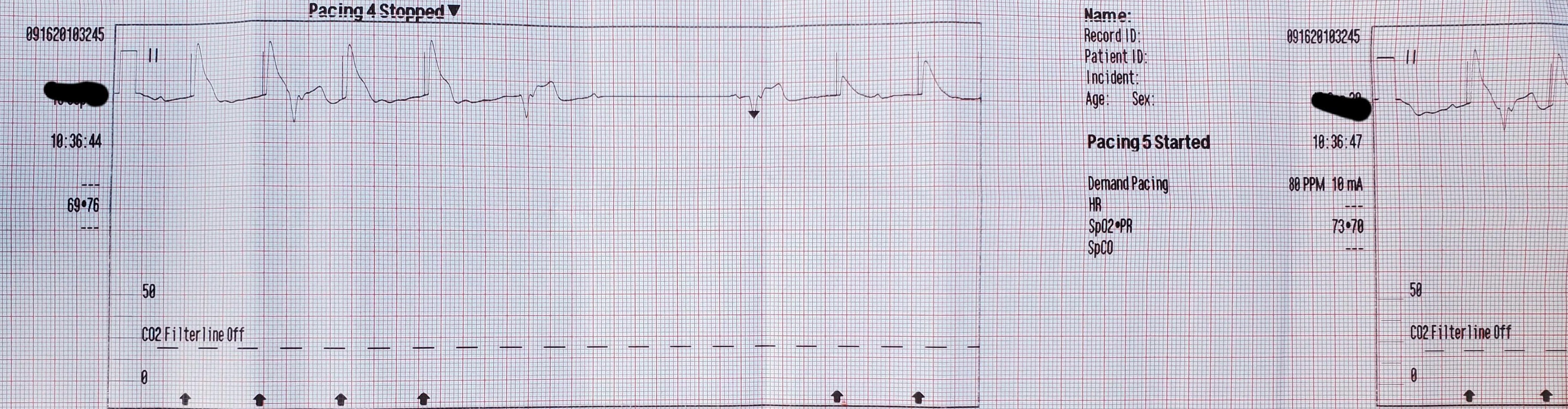
In back of the ambulance 4 lead shows sinus bradycardia @ 30 with a palpable carotid pulse still , BVM and OPA intiated. Partner is placing pt on pads, BP, SP02, ETC02 and hooking up a 12 lead,
Im working on IV access simultaneously (2 attempts failed) and jump to an IO which is successful. 12 lead shows antero-lateral infarct with tombstone elevations in 1, AVL, V3,4,5,6. We actually get a BP somehow of 117/60, Skins are Literally Grey and cool, Pupils PERRL @ 3mm, lungs Clear, Fire gets a blood sugar which is unremarkable, Narcan considered but not given as this clearly appears cardiac in nature. Prior history of Bacterial pneumonia and thats about all.
By the time my initial vitals are back and pt is fully on the monitor he's coded and Now in PEA.
CPR Started, No shocks given or advised. No epi able to be given as transport time to the Hospital less than 2 minutes and Doing 1 handed CPR while giving radio reports.
SO i feel like i Could have POSSIBLY started pacing him sooner, maybe i just feel guilty though. Do you think if i had of started pacing him sooner it could have prevented him coding?
Cause the other half of me feels like half of the pt's heart completely lost blood flow and he was sorta ****ed, and even if i WAS able to pace him before he coded, i would have ended up pretty quickly pacing a dead person.
Anyways, Hospital got back ROSC several times but ultimately called it as they were just epi-pulses, and ER staff said theyre 12 lead was also Just devastatingly bad / essentially no hope for the guy.
Questions? Anything you would have done differently?
60yo M, A&0X4 GCS15 called for shortness of breath. Pt seems almost like a drug induced sort of Presentation, Rolling around on the bed really just "playing it up" but am on the fence weather he's just in SEVERE distress or playing it up. Very agressive and non-compliant with assessment questions, Overall home enviornment and family members suport this suspicon as well.
initial vital signs are unable to be obtained due to pt LITERALLY constantly moving and rolling around and yelling.
We get him on a tarp and carry out, and He goes limp and GCS3 with agonal respirations like 10 seconds before getting him onto the gurney.
In back of the ambulance 4 lead shows sinus bradycardia @ 30 with a palpable carotid pulse still , BVM and OPA intiated. Partner is placing pt on pads, BP, SP02, ETC02 and hooking up a 12 lead,
Im working on IV access simultaneously (2 attempts failed) and jump to an IO which is successful. 12 lead shows antero-lateral infarct with tombstone elevations in 1, AVL, V3,4,5,6. We actually get a BP somehow of 117/60, Skins are Literally Grey and cool, Pupils PERRL @ 3mm, lungs Clear, Fire gets a blood sugar which is unremarkable, Narcan considered but not given as this clearly appears cardiac in nature. Prior history of Bacterial pneumonia and thats about all.
By the time my initial vitals are back and pt is fully on the monitor he's coded and Now in PEA.
CPR Started, No shocks given or advised. No epi able to be given as transport time to the Hospital less than 2 minutes and Doing 1 handed CPR while giving radio reports.
SO i feel like i Could have POSSIBLY started pacing him sooner, maybe i just feel guilty though. Do you think if i had of started pacing him sooner it could have prevented him coding?
Cause the other half of me feels like half of the pt's heart completely lost blood flow and he was sorta ****ed, and even if i WAS able to pace him before he coded, i would have ended up pretty quickly pacing a dead person.
Anyways, Hospital got back ROSC several times but ultimately called it as they were just epi-pulses, and ER staff said theyre 12 lead was also Just devastatingly bad / essentially no hope for the guy.
Questions? Anything you would have done differently?