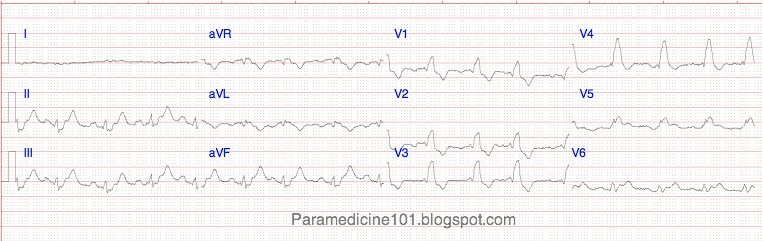
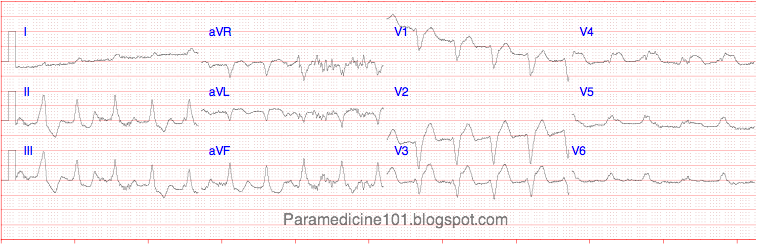
clibb, I would agree that it looks like a first degree block, or possibly even a wenckebach(hard to tell without seeing a couple more seconds) after the patient converted.
If you look at lead II.
It goes from V-Tach to Cuplet PVCs. Then the T waves aren't consistent at all. ST segment looks normal or I would think MI.
If you go to the fourth T-P waves after the V-tach on Lead II the T and P waves and how it the line declines is something I'd be worried about.
And then it looks like it leads into the heart blocks.
On lead I and lead III, I would totally agree with the Wenckebach.
These are fun. I have like 100 strips from my EKG class if you guys want me to post them.