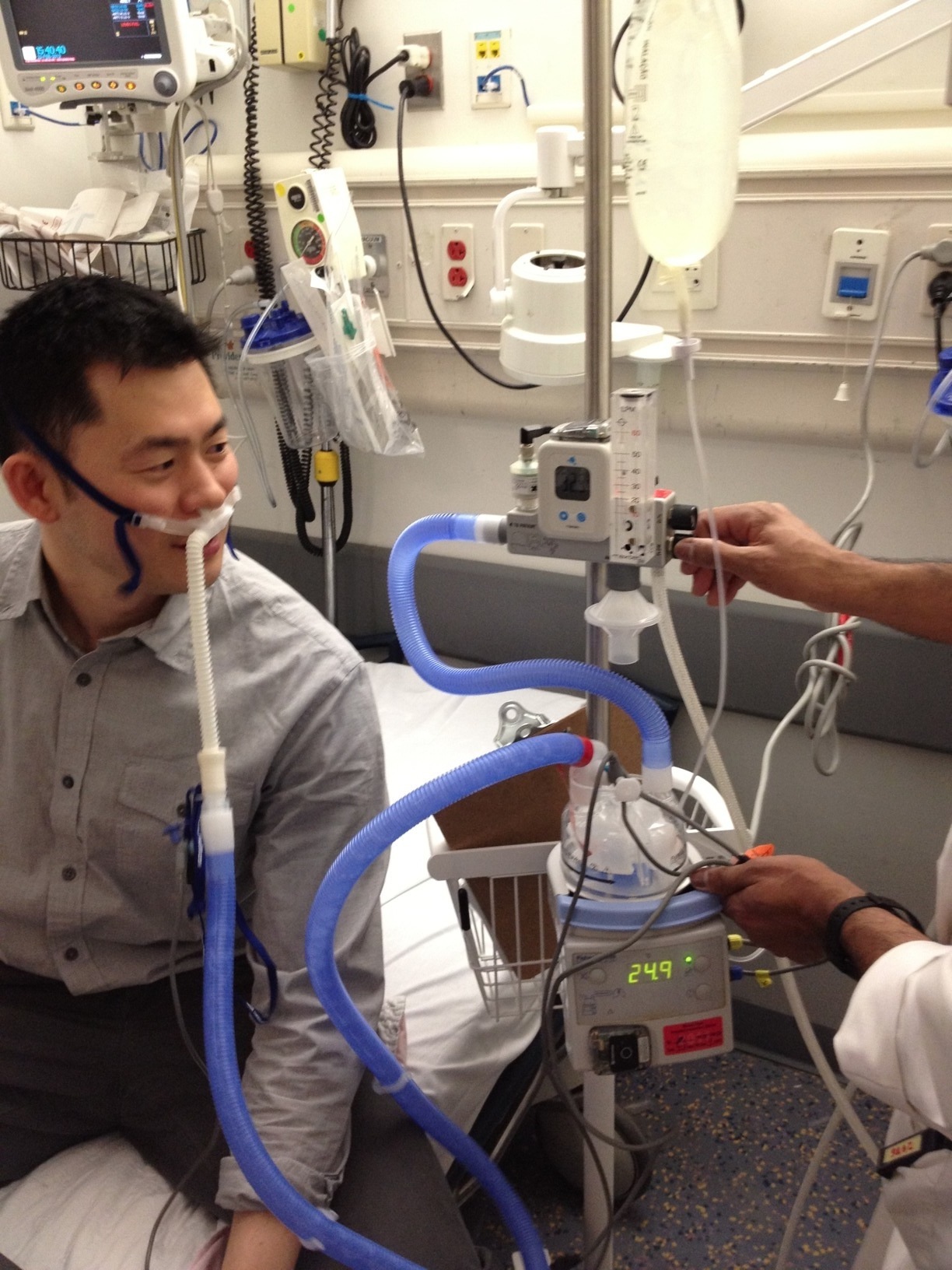
The citation about adding canulas to oxygen masks seemed to me to make it clear they were using standard cannulas, not special ones.
I am unable to find any studies comparing effective flow versus indicated flow in cannulas pushed beyond their rated LPM's.
Are these rates being measured by a Bourdon, Pitot, or other type gauge? Or using a regulator with dents ("clicks") in the flow meter knob which indicate arbitrarily what LPM is being issued but not actually being measured?
Bourdon style: can indicate increase in flow rate if there is an obstruction because it operates on the pressure in the curved measuring tube connected to the dial, like an aneroid sphyg. "Obstruction" in this case could be turbulence in the tubing or the nasopharynx or elsewhere.
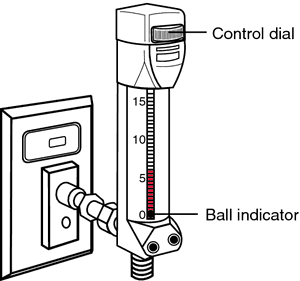
Pitot style indicates true flow if it is close to upright and interior of the vertical chamber is dry.
Precalibrated fixed-flow style : works only if the designated delivery style is used (cannula, regular mask, non-rebreather mask, rescue mask with headband and O2 port) because it does not truly measure flow rate.
Bourdon and fixed-flow regulators might indicate a higher flow rate when the actual flow rate at the patient was the same or only very slightly raised because of intracannular turbulence (or other obstructions) .
Like taking a police whistle and hooking it up to an air compressor and expecting to get a siren but all you get is a crummy dog whistle, if anything.
I'm going to try to find more about high flow cannulas.