ERDoc
Forum Asst. Chief
- 546
- 616
- 93
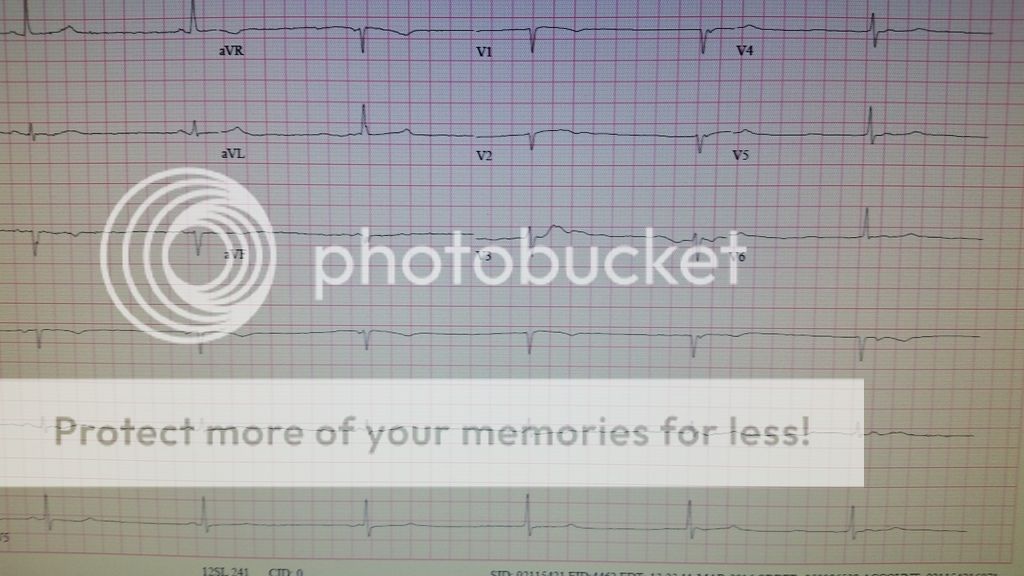
You are called to the residence of a 78y/o female how says about an hour before she called she had a sudden onset of feeling light headed, like she was going to pass out. She says she can't stand because it makes her feel worse. She also has a substernal tightness and shortness of breath.
On exam, she is noted to be wearing her normal glasses and then dark glasses over them. She is holding her head and moaning. Your partner gets a set of vitals: HR 32 BP 70/32 RR 22 Sat 96%RA.
On exam, she is noted to be wearing her normal glasses and then dark glasses over them. She is holding her head and moaning. Your partner gets a set of vitals: HR 32 BP 70/32 RR 22 Sat 96%RA.