Anjel
Forum Angel
- 4,548
- 302
- 83
Dispatched to an independent living facility for a fall secondary to a possible heart attack at 0530.
Arrived on scene to find an 89 year old male patient laying supine on the floor of his bathroom. Pt A&Ox4 and in no apparent distress. There is a good size pooling of blood against the wall when you first walk in, that is coagulated. Blood running down the wall as well. Pt has a 2 inch laceration to the top of his head that is still bleeding, and bright red blood coming from his right ear. Unable to find laceration. Pt had dried blood all over his face as well.
Pt states the last thing he remembers was at 0130 he got up to go to the bathroom. He doesn't remember falling. The next thing he does remember was rolling over to his pull cord by the toilet and calling for help- 4 hours later. He says his defibrillator went off 2 times during the night and he thinks he is having a heart attack. He denies any chest pain or difficulty in breathing. He does have cervical tenderness. Pt is on Plavix.
Hx: Pacemaker/defib, CHF, anxiety, diabetes.
Meds: Plavix, Asa, Aldactone, xanax
So here is the 12 lead. I tried everything to get the limb leads to read better and they wouldn't. He was skin and bones so I don't know what the issue was.
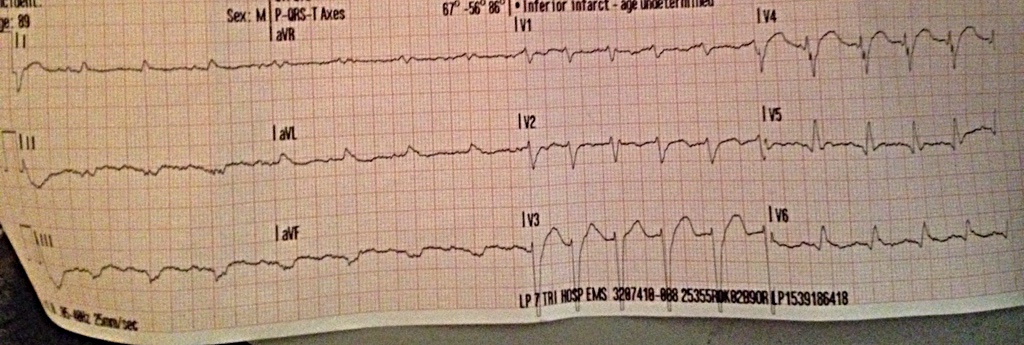
I was confused as to what was going on in V3 and V4. I don't see any pacer spikes, and my limb leads weren't very helpful.
Idk what say you guys? What would your course of treatment be?
Arrived on scene to find an 89 year old male patient laying supine on the floor of his bathroom. Pt A&Ox4 and in no apparent distress. There is a good size pooling of blood against the wall when you first walk in, that is coagulated. Blood running down the wall as well. Pt has a 2 inch laceration to the top of his head that is still bleeding, and bright red blood coming from his right ear. Unable to find laceration. Pt had dried blood all over his face as well.
Pt states the last thing he remembers was at 0130 he got up to go to the bathroom. He doesn't remember falling. The next thing he does remember was rolling over to his pull cord by the toilet and calling for help- 4 hours later. He says his defibrillator went off 2 times during the night and he thinks he is having a heart attack. He denies any chest pain or difficulty in breathing. He does have cervical tenderness. Pt is on Plavix.
Hx: Pacemaker/defib, CHF, anxiety, diabetes.
Meds: Plavix, Asa, Aldactone, xanax
So here is the 12 lead. I tried everything to get the limb leads to read better and they wouldn't. He was skin and bones so I don't know what the issue was.
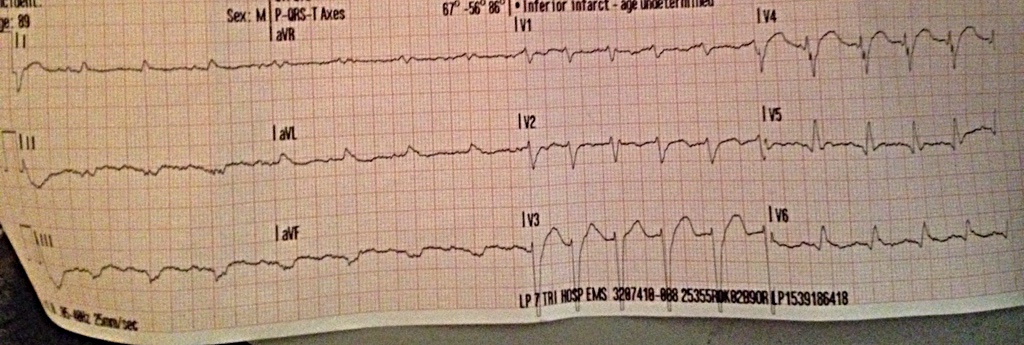
I was confused as to what was going on in V3 and V4. I don't see any pacer spikes, and my limb leads weren't very helpful.
Idk what say you guys? What would your course of treatment be?
