At my night shift on a ILS service (me-EMTB and a pre-hospital RN), we received a call at 7 am for a rural area. A 50 year old man with weakness, diaphoresis, and chest pain that radiates to the back and left arm. When we arrived, we found him lying in bed, being assisted by local firefighters.
Medical history: Familial hypercholesterolemia and hypertension. Denies allergies. Meds: sinvastatin, hydrochlorothiazide+irbesartam , vitamin supplements and echinacea.
Vitals:
Pulse: 70 and regular
BP: 110/70
RR: 22 unlabored, simetric and regular
Pain: 7/10 -> started 1 hour ago
Pulse ox: 96% on 2 liters by nasal cannula
Physical Examination:
Skin is pale and wet. Breath sounds are normal. Heart tones: S1 and S2 present in all fields, without murmurs.
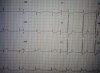
12-lead ECG was performed, and shows STEMI.
The nurse started an IV and administered 5 mg of morphine sulfate, SL nitro, ASA PO. The hospital with cath lab has ETA of 45 minutes and the small ER 20 minutes. We and the medical supervisor, decided to transport to the hospital with cath lab.
During transport, the patient went into cardiac arrest (rhythm was v-fib). We stop the ambulance and starded the ILS algorithm. ALS unit is unavailable. After 25 minutes (shocks, drugs, entubation ET), the rhythm was assystole, and medical supervisor ordered transport to the small ER. Upon arrival, he was pronounced dead.
What did you do differently?
Would have continued the resuscitation procedures in the field?
NOTE: We carry fibrinolytics in the ambulance, but the medical supervisor denied fibrinolysis.
Medical history: Familial hypercholesterolemia and hypertension. Denies allergies. Meds: sinvastatin, hydrochlorothiazide+irbesartam , vitamin supplements and echinacea.
Vitals:
Pulse: 70 and regular
BP: 110/70
RR: 22 unlabored, simetric and regular
Pain: 7/10 -> started 1 hour ago
Pulse ox: 96% on 2 liters by nasal cannula
Physical Examination:
Skin is pale and wet. Breath sounds are normal. Heart tones: S1 and S2 present in all fields, without murmurs.
12-lead ECG was performed, and shows STEMI.
The nurse started an IV and administered 5 mg of morphine sulfate, SL nitro, ASA PO. The hospital with cath lab has ETA of 45 minutes and the small ER 20 minutes. We and the medical supervisor, decided to transport to the hospital with cath lab.
During transport, the patient went into cardiac arrest (rhythm was v-fib). We stop the ambulance and starded the ILS algorithm. ALS unit is unavailable. After 25 minutes (shocks, drugs, entubation ET), the rhythm was assystole, and medical supervisor ordered transport to the small ER. Upon arrival, he was pronounced dead.
What did you do differently?
Would have continued the resuscitation procedures in the field?
NOTE: We carry fibrinolytics in the ambulance, but the medical supervisor denied fibrinolysis.