Called by an Sherriff for a sick person at a store.
31 y/o M supine on the ground. A&Ox4, very pale and diaphoretic. Pt was shopping and reported a syncopal episode with a sudden onset of abdominal pain, nausea, and vomiting.
Pt reports sharp, periumbilical pain and has difficulty remaining still or finding a position of comfort. Pt required a 2 person assist to the stretcher and unable to support himself. No recent illness, alcohol/drug use, or other recent symptoms.
Hx: Gallbladder problems and depression
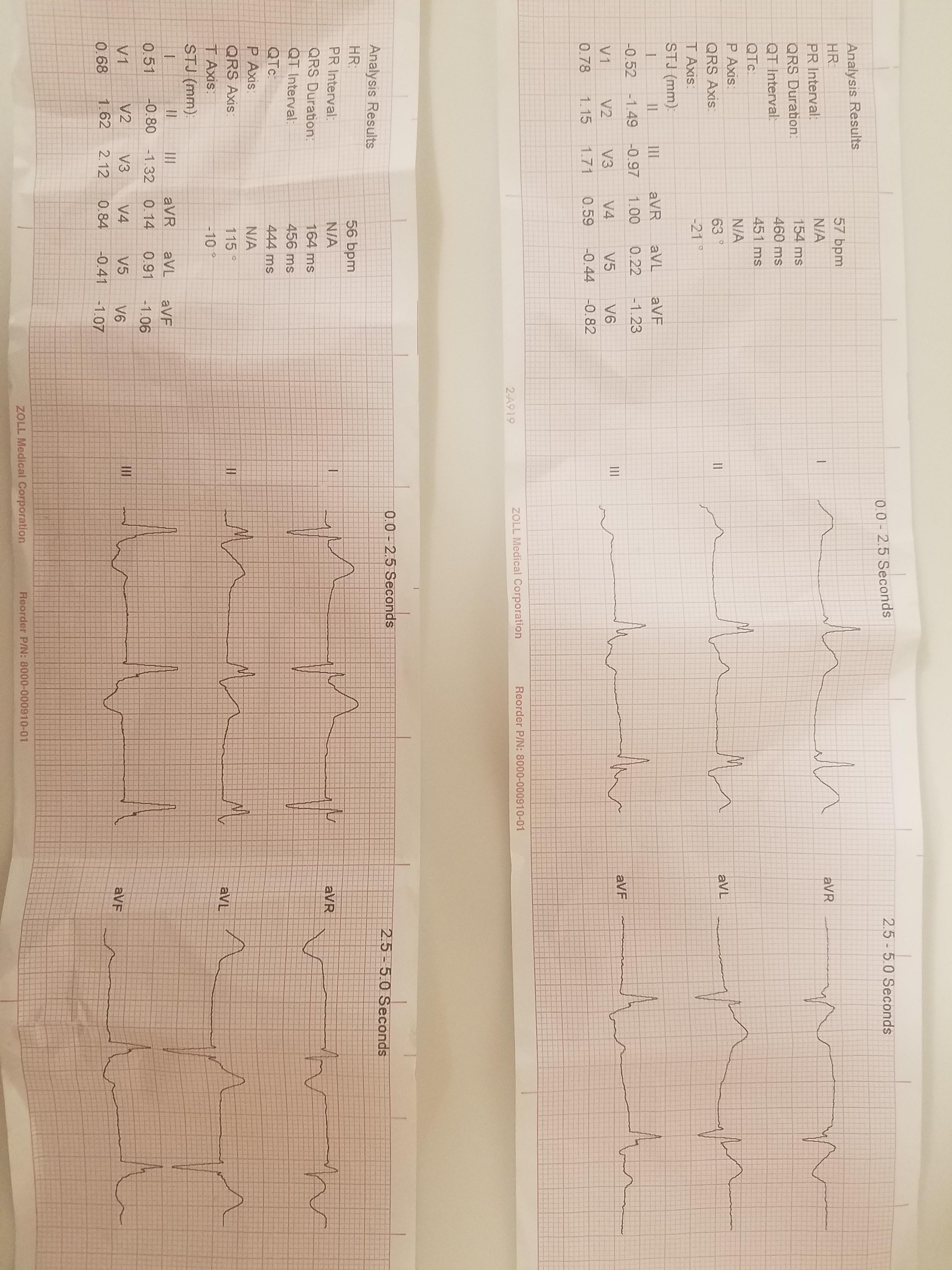
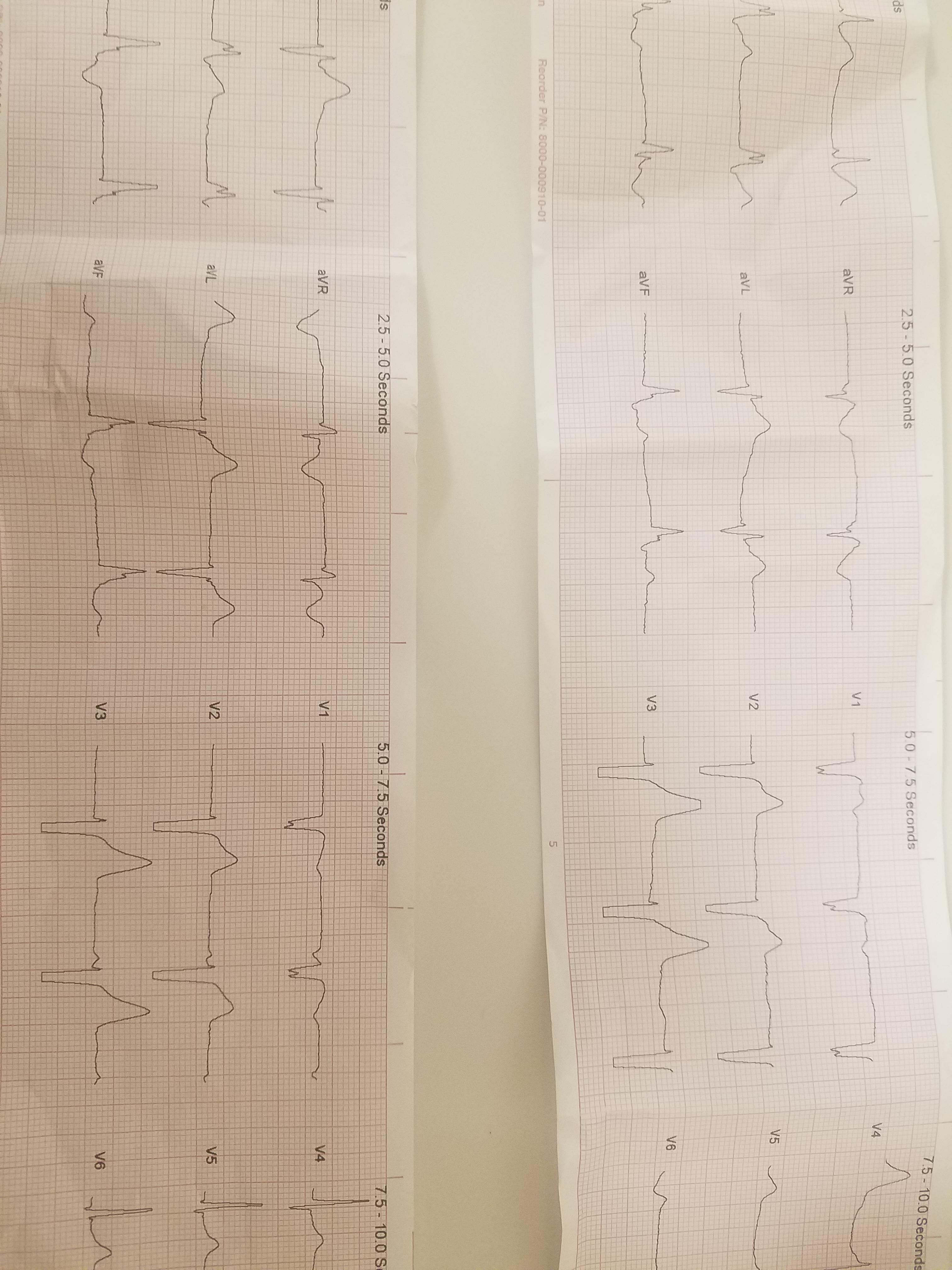
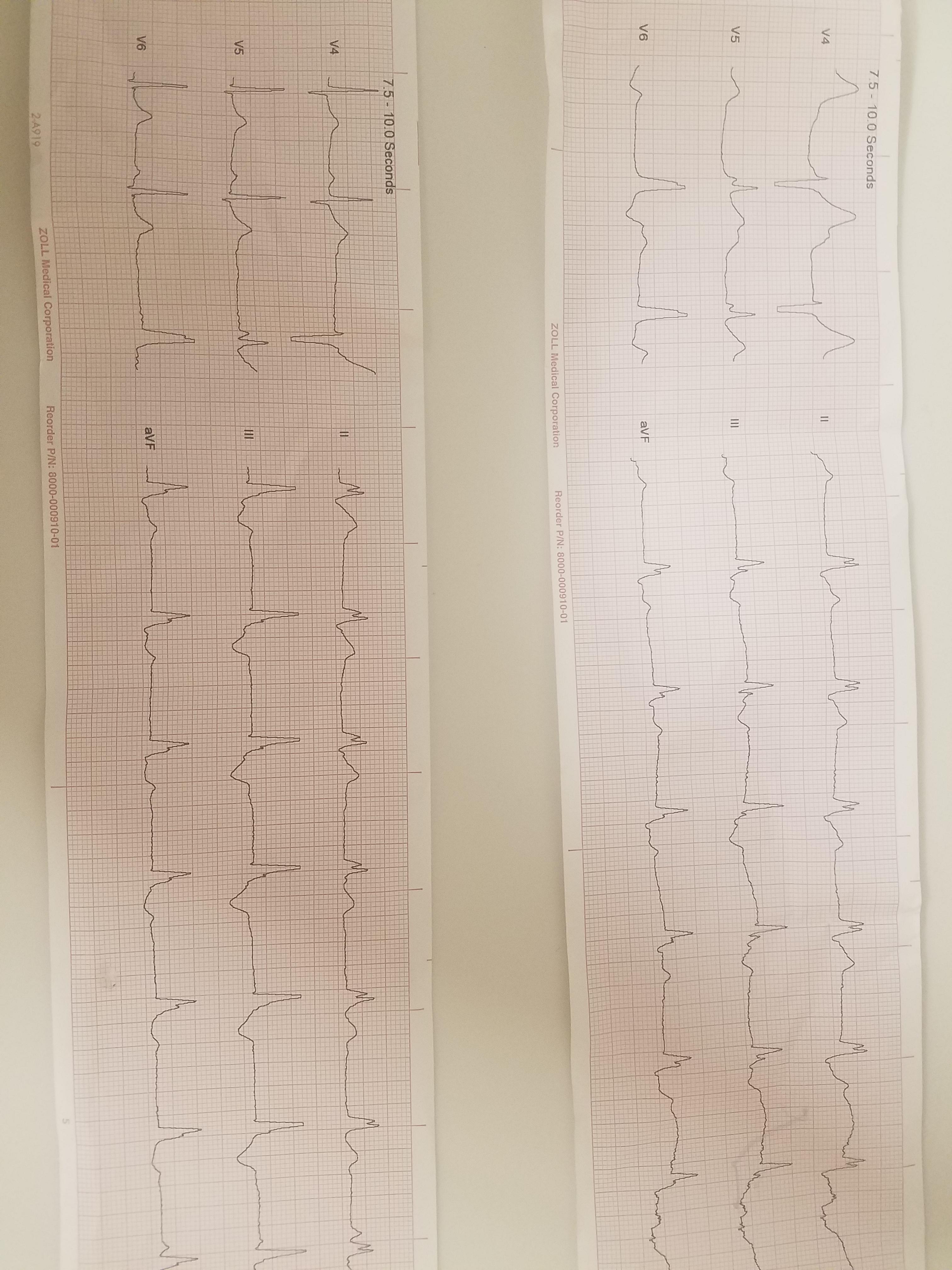
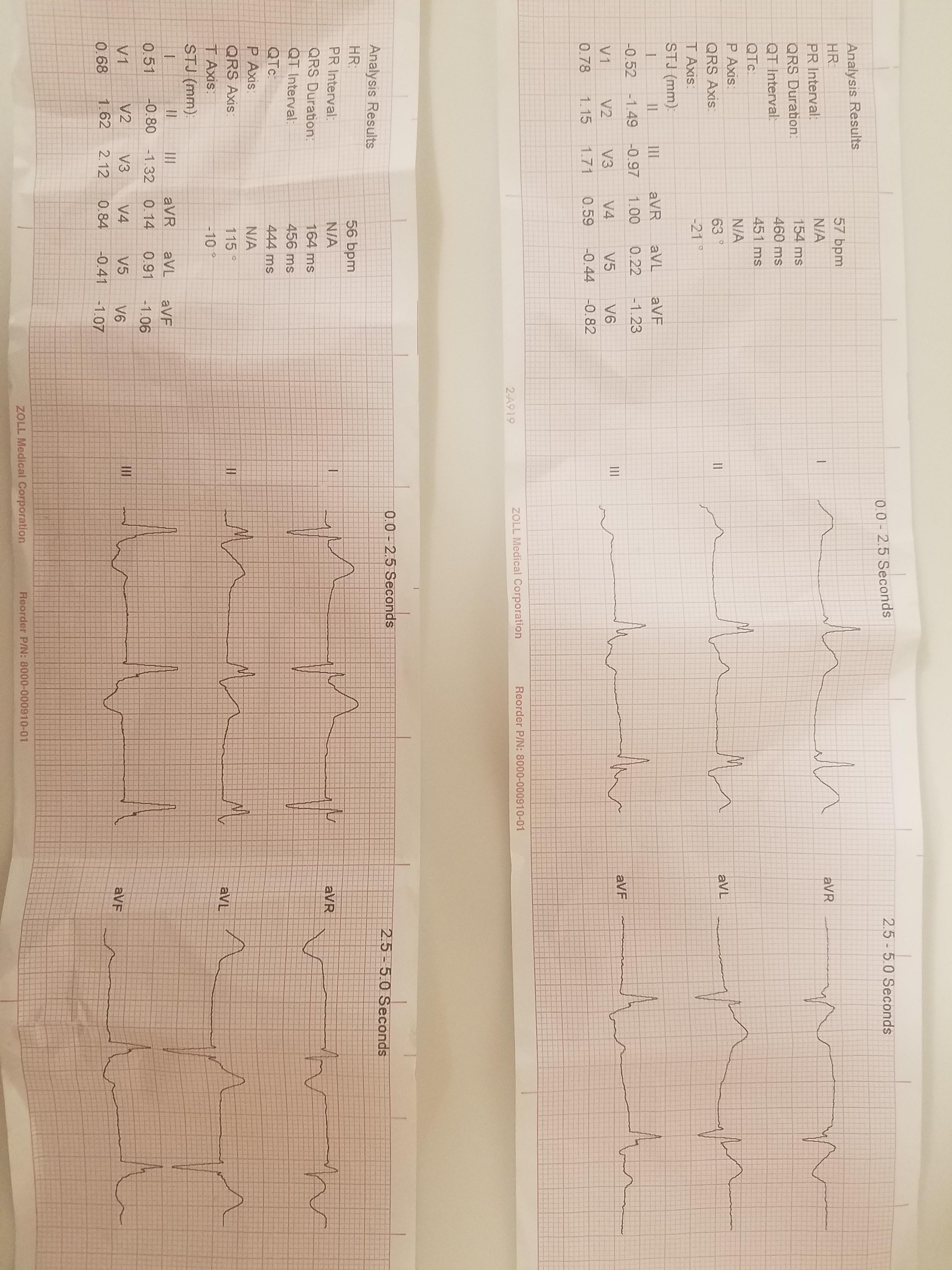
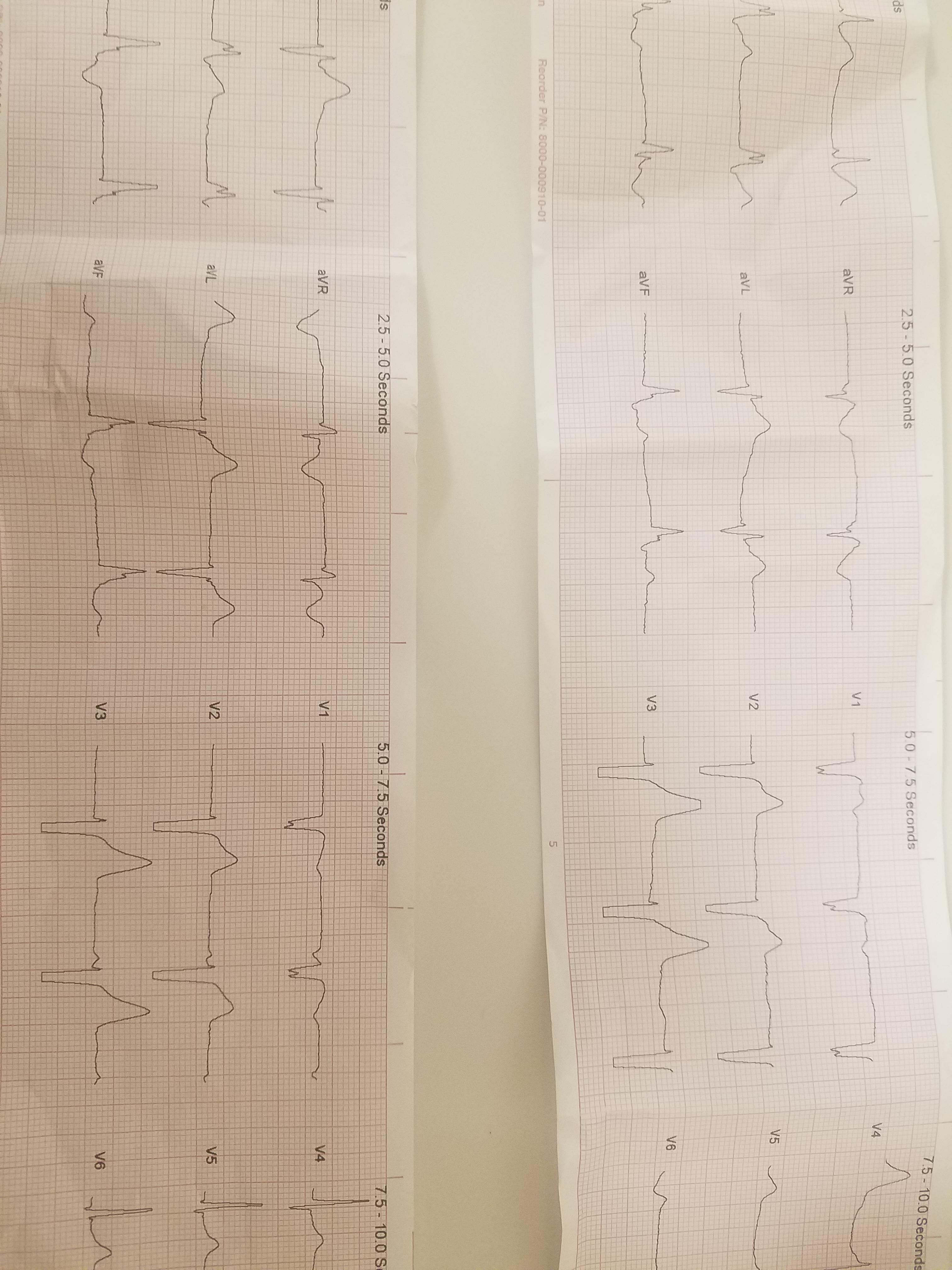
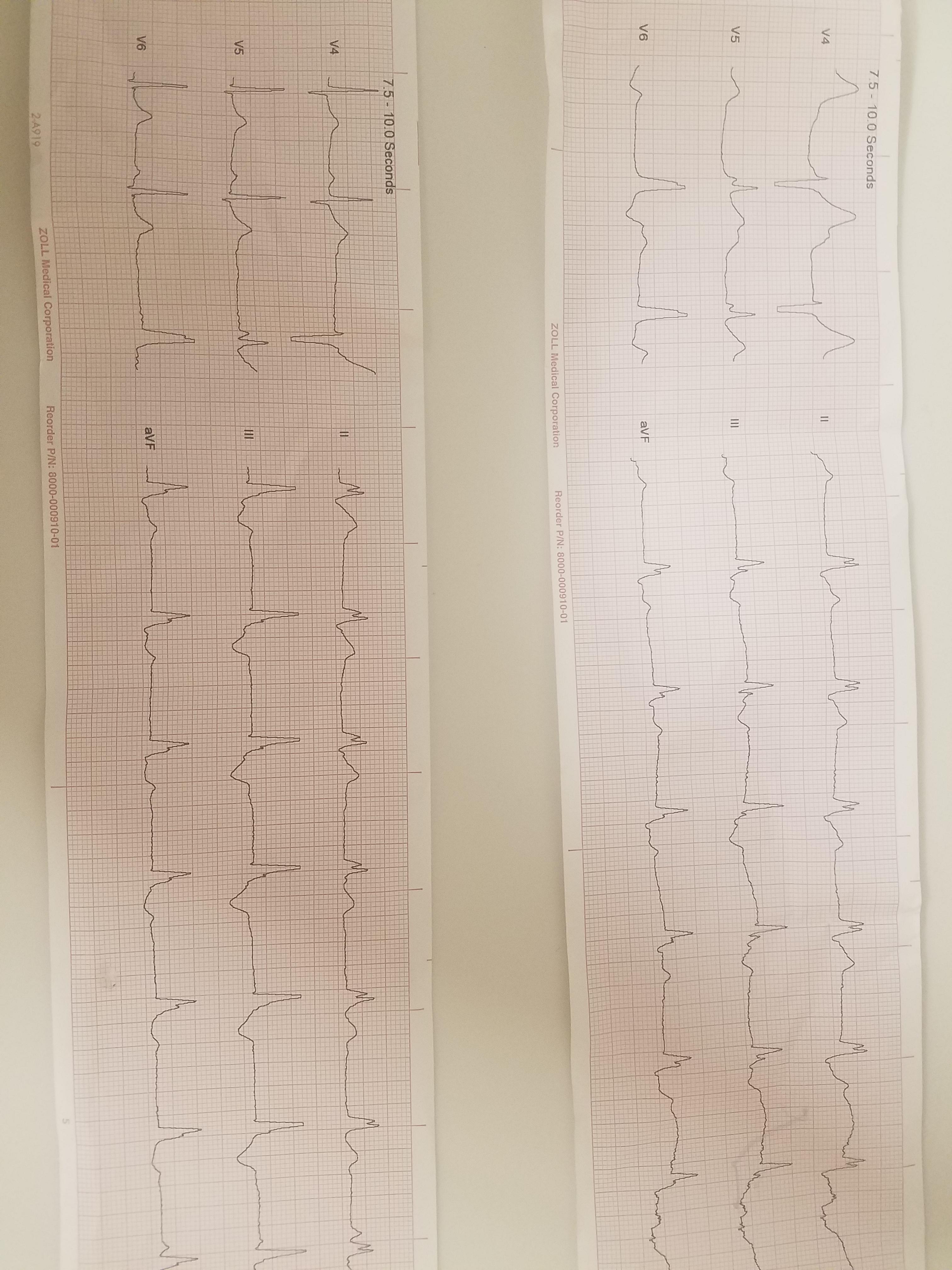
Vx: HR 50's as noted above, SpO2 96%, BP 100's/60's.
Tx: 4mg Zofran and 100mcg of Fentanyl.
( I was not AIC and drove to the hospital, so I don't really have any good reassessment answers, but it was a very short trip so there likely isn't anything significant to note. At least not that I am aware of)
31 y/o M supine on the ground. A&Ox4, very pale and diaphoretic. Pt was shopping and reported a syncopal episode with a sudden onset of abdominal pain, nausea, and vomiting.
Pt reports sharp, periumbilical pain and has difficulty remaining still or finding a position of comfort. Pt required a 2 person assist to the stretcher and unable to support himself. No recent illness, alcohol/drug use, or other recent symptoms.
Hx: Gallbladder problems and depression
Vx: HR 50's as noted above, SpO2 96%, BP 100's/60's.
Tx: 4mg Zofran and 100mcg of Fentanyl.
( I was not AIC and drove to the hospital, so I don't really have any good reassessment answers, but it was a very short trip so there likely isn't anything significant to note. At least not that I am aware of)