Our department recently had a trauma call. From what we have heard the call went terribly wrong. We have a lot of concerns, and questions that could effect patient care in the future, but the medic who handled the call is our boss and he isn't giving any information. So I thought I would toss out some of the issues and see what everyone thinks. I guess first I should make sure I can post anything. Am I allowed to post details of the call? I know I can't post name or anything, but can I post about the call in detail?
Navigation
Install the app
How to install the app on iOS
Follow along with the video below to see how to install our site as a web app on your home screen.
Note: This feature may not be available in some browsers.
More options
Style variation
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Trauma arrest, should CPR be stopped in the field?
- Thread starter med109
- Start date
- 9,736
- 1,174
- 113
As long as it isn't identifying to the patient you can post it. Be nonspecific about locations and what not.
For what it's worth we rarely transport traumatic arrests.
For what it's worth we rarely transport traumatic arrests.
Last edited by a moderator:
TransportJockey
Forum Chief
- 8,623
- 1,676
- 113
Traumatic arrests are just a warm dear body. We don't transport any arrests here unless there is mitigating circumstances. No point.
Ok here goes...
My boss is an intermediate and he had a driver (not even basic certified) with him. They knew CPR was in progress before they left the station, He could have had a helicopter or another ALS rig on scene within minutes but chose not to. Officers on scene started CPR but then noticed a pulse so they stopped. When they checked again there was no pulse and CPR was continued. EMS couldn't get the ambulance to the patient as he was at the top of an adobe hill, so they loaded a board and the jump kit into an officers truck and rode up. They quickly boarded the patient, and continued CPR. Well actually the driver did CPR while the medic called the Dr for orders. I am not sure what he told the Dr, but the Dr said it was ok to stop working the patient. So they did. I could list our protocol for stopping CPR in the field but I won't. They do say that you can't stop if there was preceding trauma, and if drugs or alcohol are suspected. The patient was ETOH, my boss said he was vomitting beer. It also says you have to have an airway, IV, and do 3 cycles of rhythm appropriate meds. NONE of those were done. So they unloaded the patient from the officers truck, and set him on the ground to wait for the coroner. The bystanders (patients family and friends) asked if they could please put him in the ambulance so they didn't have to see his body laying there. My boss told them NO, he didn't want the mess (vomit and dirt, the patients wasn't bleeding at all) in the rig, and he didn't want to have the rig out of service should another call come in. So they kept him on our back board and loaded him into the back of the officers truck again. WHere the patient vomitted 2 more times! The bystanders were mortified.
So what do you think? We are always taught to call the Dr and let him take the fall if there is one to take, but shouldn't the medic take some fall here? He didn't even follow our protocol. This was a new ER Dr that he talked to, and she had never given medical direction to EMS before.
Would you have stopped CPR in the field like that?
There was no paramedic involved in the call, our protocols say a paramedic has to be involved in the efforts. I always thought a paramedic could stop CPR in the field with medical direction, but only a paramedic.
Any other thought or ideas on what should have happened during the call. Our department mainly has basics, and they can have ALS to the scene pretty quick. But what would you advise a crew of basics to do?
My boss is an intermediate and he had a driver (not even basic certified) with him. They knew CPR was in progress before they left the station, He could have had a helicopter or another ALS rig on scene within minutes but chose not to. Officers on scene started CPR but then noticed a pulse so they stopped. When they checked again there was no pulse and CPR was continued. EMS couldn't get the ambulance to the patient as he was at the top of an adobe hill, so they loaded a board and the jump kit into an officers truck and rode up. They quickly boarded the patient, and continued CPR. Well actually the driver did CPR while the medic called the Dr for orders. I am not sure what he told the Dr, but the Dr said it was ok to stop working the patient. So they did. I could list our protocol for stopping CPR in the field but I won't. They do say that you can't stop if there was preceding trauma, and if drugs or alcohol are suspected. The patient was ETOH, my boss said he was vomitting beer. It also says you have to have an airway, IV, and do 3 cycles of rhythm appropriate meds. NONE of those were done. So they unloaded the patient from the officers truck, and set him on the ground to wait for the coroner. The bystanders (patients family and friends) asked if they could please put him in the ambulance so they didn't have to see his body laying there. My boss told them NO, he didn't want the mess (vomit and dirt, the patients wasn't bleeding at all) in the rig, and he didn't want to have the rig out of service should another call come in. So they kept him on our back board and loaded him into the back of the officers truck again. WHere the patient vomitted 2 more times! The bystanders were mortified.
So what do you think? We are always taught to call the Dr and let him take the fall if there is one to take, but shouldn't the medic take some fall here? He didn't even follow our protocol. This was a new ER Dr that he talked to, and she had never given medical direction to EMS before.
Would you have stopped CPR in the field like that?
There was no paramedic involved in the call, our protocols say a paramedic has to be involved in the efforts. I always thought a paramedic could stop CPR in the field with medical direction, but only a paramedic.
Any other thought or ideas on what should have happened during the call. Our department mainly has basics, and they can have ALS to the scene pretty quick. But what would you advise a crew of basics to do?
TransportJockey
Forum Chief
- 8,623
- 1,676
- 113
I'm on my phone so I'll only address the non paramedic calling a course part... as an EMT-I I called several arrests. An asystolic code can be worked adequately by an intermediate. But it sounds like the call was handled poorly. Although he was right about now taking a truck out of service.
NomadicMedic
I know a guy who knows a guy.
- 12,248
- 7,030
- 113
Was this even a traumatic arrest? What was the situation leading to arrest? Fall? MVA?
A "traumatic arrest" usually involves injuries incompatible with life.
A "traumatic arrest" usually involves injuries incompatible with life.
Was this even a traumatic arrest? What was the situation leading to arrest? Fall? MVA?
A "traumatic arrest" usually involves injuries incompatible with life.
OOOPS how did I forget that lol. It was a dirtbike accident. Maybe I choose my wording wrong, it was a trauma, and appears he went into cardiac arrest. I say appears because the officers that checked for pulse arn't very trained in first aid and it seems weird that they found a pulse then didn't find a pulse. Also I say appears because they never put a monitor on the patient.
Anjel
Forum Angel
- 4,548
- 302
- 83
I call BS. No way a doctor is giving a pronouncement without a strip.
NomadicMedic
I know a guy who knows a guy.
- 12,248
- 7,030
- 113
Yeah, this whole thing sounds like troll bait to me.
socalmedic
Mediocre at best
- 789
- 8
- 18
I dont need a strip to call a traumatic arrest. greater than 20 min from time of initial pulselessness by EMS to trauma center arrival = DOA. I would not have even put him of a board. I would have called him where he lied, and assisted PD to load the body into THEIR truck if asked because I doubt the coroner is going to walk up to to body.
the HELO is not needed, they wont fly an arrest. a Paramedic is not needed as an intermediate can do everything I would have done for this patient (if the intermediate has a monitor)
sounds like your service does not get many arrests. maby it is time to start drilling on the less frequent calls.
the HELO is not needed, they wont fly an arrest. a Paramedic is not needed as an intermediate can do everything I would have done for this patient (if the intermediate has a monitor)
sounds like your service does not get many arrests. maby it is time to start drilling on the less frequent calls.
Bieber
Forum Crew Member
- 93
- 0
- 0
Everything sounds good so far. No need to waste a chopper on a patient that has basically zero chance of survival.Ok here goes...
My boss is an intermediate and he had a driver (not even basic certified) with him. They knew CPR was in progress before they left the station, He could have had a helicopter or another ALS rig on scene within minutes but chose not to. Officers on scene started CPR but then noticed a pulse so they stopped. When they checked again there was no pulse and CPR was continued. EMS couldn't get the ambulance to the patient as he was at the top of an adobe hill, so they loaded a board and the jump kit into an officers truck and rode up. They quickly boarded the patient, and continued CPR. Well actually the driver did CPR while the medic called the Dr for orders. I am not sure what he told the Dr, but the Dr said it was ok to stop working the patient. So they did.
Don't know what your policy is, but once we have a patient in the back of the truck if we terminate we're out of service until the coroner arrives.I could list our protocol for stopping CPR in the field but I won't. They do say that you can't stop if there was preceding trauma, and if drugs or alcohol are suspected. The patient was ETOH, my boss said he was vomitting beer. It also says you have to have an airway, IV, and do 3 cycles of rhythm appropriate meds. NONE of those were done. So they unloaded the patient from the officers truck, and set him on the ground to wait for the coroner. The bystanders (patients family and friends) asked if they could please put him in the ambulance so they didn't have to see his body laying there. My boss told them NO, he didn't want the mess (vomit and dirt, the patients wasn't bleeding at all) in the rig, and he didn't want to have the rig out of service should another call come in. So they kept him on our back board and loaded him into the back of the officers truck again. WHere the patient vomitted 2 more times! The bystanders were mortified.
Sounds like the EMT in question used critical thinking skills to determine the most appropriate course of action rather than blindly follow a cookbook. What's wrong with that?So what do you think? We are always taught to call the Dr and let him take the fall if there is one to take, but shouldn't the medic take some fall here? He didn't even follow our protocol. This was a new ER Dr that he talked to, and she had never given medical direction to EMS before.
I'd never have started CPR. Our treatment for traumatic arrest is to open the airway and ventilate via BVM, assess for and treat pneumothoraces, and confirm asystole. If all of those things have been done, we terminate all efforts.Would you have stopped CPR in the field like that?
EMT's can follow medical direction as well. It may have been good to involve a paramedic, but I doubt it would have made a difference. Survival rates for traumatic arrest are horrible.There was no paramedic involved in the call, our protocols say a paramedic has to be involved in the efforts. I always thought a paramedic could stop CPR in the field with medical direction, but only a paramedic.
Any other thought or ideas on what should have happened during the call. Our department mainly has basics, and they can have ALS to the scene pretty quick. But what would you advise a crew of basics to do?
- 9,736
- 1,174
- 113
I call BS. No way a doctor is giving a pronouncement without a strip.
Why? Our docs will on traumatic arrests, we still generally will put the monitor on them just to confirm but it's not a requirement.
"Doc I'm 15 minutes out with a 26 yo female in cardiac arrest secondary to being ejected during a vehicle rollover, may we terminate efforts?" "Yes, T.O.D. xxxx"
People DON'T survive traumatic arrests. It just doesn't happen. Everyone once in a million it happens.
I don't see any issue with how he handled the call other than originally boarding the pt and moving them. Could've handled family better as well.
My .02 but walked up and found a dirtbiker in arrest after a crash we doing BLS and I'm calling for orders. We don't transport dead people.
I wouldn't have put them in my truck either, like others have said you just made your ambulance part of the crime scene if you do that and you're going to be stuck for a while.
NomadicMedic
I know a guy who knows a guy.
- 12,248
- 7,030
- 113
Either I'm missing something or you are. How does "everything sounds good" in this scenario?
There is no clear presentation of what the cause of this arrest was. If the original poster had mentioned that the patient was decapitated, had a head that was smashed in from the motorcycle landing on it, had A dismembered arm and full thickness burns over 90% of his body… Then I could see not working or early termination of this arrest.
But, it's presented as a "dirtbike accident" no specific mention of obvious signs of trauma or injury incompatible with life. And I'm sorry, there is no way in hell I would ever call a cardiac arrest, trauma or not, without an asystole strip.
I think the biggest issue here is that the protocol specifically calls for a paramedic to be involved in the pronouncement or attempted resuscitation of the trauma arrest. That did not happen. Also, never mind the doc not seeing the asystole strip, they never put the monitor on.
I think we need more information from the original poster and we need to see a copy of those protocols. If there is a protocol violation, the EMT that pronounced that arrest should be disciplined.
Not to mention the awful customer service.
There is no clear presentation of what the cause of this arrest was. If the original poster had mentioned that the patient was decapitated, had a head that was smashed in from the motorcycle landing on it, had A dismembered arm and full thickness burns over 90% of his body… Then I could see not working or early termination of this arrest.
But, it's presented as a "dirtbike accident" no specific mention of obvious signs of trauma or injury incompatible with life. And I'm sorry, there is no way in hell I would ever call a cardiac arrest, trauma or not, without an asystole strip.
I think the biggest issue here is that the protocol specifically calls for a paramedic to be involved in the pronouncement or attempted resuscitation of the trauma arrest. That did not happen. Also, never mind the doc not seeing the asystole strip, they never put the monitor on.
I think we need more information from the original poster and we need to see a copy of those protocols. If there is a protocol violation, the EMT that pronounced that arrest should be disciplined.
Not to mention the awful customer service.
Last edited by a moderator:
socalmedic
Mediocre at best
- 789
- 8
- 18
there is no way in hell I would ever call a cardiac arrest, trauma or not, without an asystole strip.
is this your protocol or just how you do it? out here I wouldnt have even carried the monitor up the hill to the patient. I would have confirmed pulselessness via apical auscultation and then informed the family.
- 9,736
- 1,174
- 113
Either I'm missing something or you are. How does "everything sounds good" in this scenario?
There is no clear presentation of what the cause of this arrest was. If the original poster had mentioned that the patient was decapitated, had a head that was smashed in from the motorcycle landing on it, had A dismembered arm and full thickness burns over 90% of his body… Then I could see not working or early termination of this arrest.
But, it's presented as a "dirtbike accident" no specific mention of obvious signs of trauma or injury incompatible with life. And I'm sorry, there is no way in hell I would ever call a cardiac arrest, trauma or not, without an asystole strip.
I think the biggest issue here is that the protocol specifically calls for a paramedic to be involved in the pronouncement or attempted resuscitation of the trauma arrest. That did not happen. Also, never mind the doc not seeing the asystole strip, they never put the monitor on.
I think we need more information from the original poster and we need to see a copy of those protocols. If there is a protocol violation, the EMT that pronounced that arrest should be disciplined.
Not to mention the awful customer service.
Fair enough, I definitely got hungup on the title of the thread.
Like I said, any arrest is going to go on the monitor unless I have a real good reason not to but by my protocols for penetrating traumatic arrests with an ETA to the TC of >10 minutes we don't need to put the monitor on.
With that said, if this scenario truly was a traumatic arrest it was more than likely going to be a blunt traumatic arrest rather then penetrating and then they have to go on the monitor.
I'm not a huge fan of "injuries incompatible with life", it's very open-ended. Technically per my protocol I can pronounce without a strip or contacting a doc on "injuries incompatible with life".
Sorry, stupid argument.
NomadicMedic
I know a guy who knows a guy.
- 12,248
- 7,030
- 113
I agree that it's a stupid argument, but it's one that keeps you from getting hung out to dry.
And all arrests going on the monitor is a protocol here, not just how I do it.
I have to find telemetric pronouncement protocol. That mentions an asystole strip specifically.
And all arrests going on the monitor is a protocol here, not just how I do it.
I have to find telemetric pronouncement protocol. That mentions an asystole strip specifically.
Last edited by a moderator:
Bieber
Forum Crew Member
- 93
- 0
- 0
Cardiac arrest following a traumatic mechanism isn't a clear presentation?Either I'm missing something or you are. How does "everything sounds good" in this scenario?
There is no clear presentation of what the cause of this arrest was.
I don't follow what you're getting at... Are you saying that trauma must be external and visible for us to base our triage/treatment on it?If the original poster had mentioned that the patient was decapitated, had a head that was smashed in from the motorcycle landing on it, had A dismembered arm and full thickness burns over 90% of his body… Then I could see not working or early termination of this arrest.
What is an asystole strip going to tell you that you can't see for yourself? Better question, what does electrical activity in the heart have to do with the viability of a patient in traumatic arrest? Do we have reason to believe that this is an electrical problem?But, it's presented as a "dirtbike accident" no specific mention of obvious signs of trauma or injury incompatible with life. And I'm sorry, there is no way in hell I would ever call a cardiac arrest, trauma or not, without an asystole strip.
Don't think for yourself. Treat the protocol, not the patient. That may not be the message you meant to present, but that's what it sounds like. And it's that kind of mentality that's lead to us worrying more about protocol violations than providing clinically sound patient care.I think the biggest issue here is that the protocol specifically calls for a paramedic to be involved in the pronouncement or attempted resuscitation of the trauma arrest. That did not happen. Also, never mind the doc not seeing the asystole strip, they never put the monitor on
I won't argue against getting more info, but the picture presented thus far paints a traumatic etiology. I'll disagree with you that the EMT should be disciplined for a protocol violation. That sends the message that EMS providers shouldn't be encouraged to think for themselves, and should instead blindly follow whatever the silly protocol says regardless of what their clinical judgment dictates.I think we need more information from the original poster and we need to see a copy of those protocols. If there is a protocol violation, the EMT that pronounced that arrest should be disciplined.
I don't disagree with you there.Not to mention the awful customer service.
Either I'm missing something or you are. How does "everything sounds good" in this scenario?
There is no clear presentation of what the cause of this arrest was. If the original poster had mentioned that the patient was decapitated, had a head that was smashed in from the motorcycle landing on it, had A dismembered arm and full thickness burns over 90% of his body… Then I could see not working or early termination of this arrest.
But, it's presented as a "dirtbike accident" no specific mention of obvious signs of trauma or injury incompatible with life. And I'm sorry, there is no way in hell I would ever call a cardiac arrest, trauma or not, without an asystole strip.
I think the biggest issue here is that the protocol specifically calls for a paramedic to be involved in the pronouncement or attempted resuscitation of the trauma arrest. That did not happen. Also, never mind the doc not seeing the asystole strip, they never put the monitor on.
I think we need more information from the original poster and we need to see a copy of those protocols. If there is a protocol violation, the EMT that pronounced that arrest should be disciplined.
Not to mention the awful customer service.
I promise guys I am not trolling. If you have no signs of penitraiting trauma, or other obvious signs of death, and you have officers say he didn't have a pulse, then he did, then he didn't, wouldn't you want to put on a monitor to see what the heck is going on before saying this guy is done? Anything else I have heard has come from bystanders so it can't be trusted, but they have said that the medic didn't even touch the patient, nor check for a pulse.
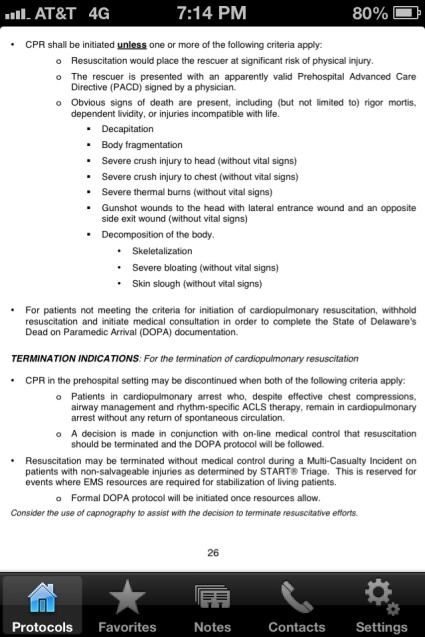
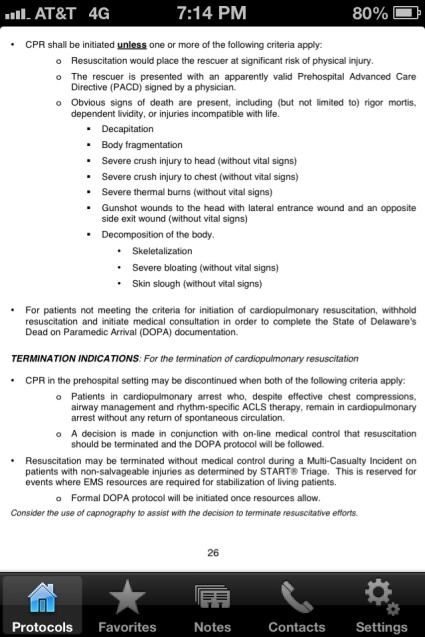
As far as our protocols go, I can try to scan them to here, or type them out. Which would be best?
TransportJockey
Forum Chief
- 8,623
- 1,676
- 113
I call BS. No way a doctor is giving a pronouncement without a strip.
Not true. I can't send steps but i get orders on a regular basis to terminate codes
Bieber
Forum Crew Member
- 93
- 0
- 0
Maybe you can give a better description of what this "dirtbike accident" consisted of? Was the patient ejected? Run over? Something else? Preceding symptoms? What were the assessment findings?I promise guys I am not trolling. If you have no signs of penitraiting trauma, or other obvious signs of death, and you have officers say he didn't have a pulse, then he did, then he didn't, wouldn't you want to put on a monitor to see what the heck is going on before saying this guy is done? Anything else I have heard has come from bystanders so it can't be trusted, but they have said that the medic didn't even touch the patient, nor check for a pulse.
As far as our protocols go, I can try to scan them to here, or type them out. Which would be best?
