Aidey
Community Leader Emeritus
- 4,800
- 11
- 38
Called for a "full arrest"
Arrive on scene and find an adult male lying on the living room floor, alive, writhing around. The ALS fire crew is attempting to assess the patient. The pt is a late 60's male who had been outside for less than 5 minutes doing physical labor. He had a witnessed collapse and was reported to be unresponsive for 1-2 minutes, before waking up and being moved back into the house. The only thing the family can tell us is that he takes nitro, and he has been complaining of back pain today, which he attributed to a pulled muscle.
The 3 lead is showing sinus tach at 144, resps of 28, the NIBP is showing error, we can't hear anything and he has no radial pulse. The SpO2 is 86% on 12 lpm. The pt is pale/grey and diaphoretic. His distal cap refill is slow, and his hands are cold. He looks bad.
In order to obtain an IV and 12 lead the patient has to be manually restrained because he will not hold still and doesn't even appear to hear you asking him to follow directions. The only thing he will say is that his chest hurts and he needs to move.
12 lead showed the following. Sorry, it is a crappy copy of a crappy tracing, but it shows enough to get the point.
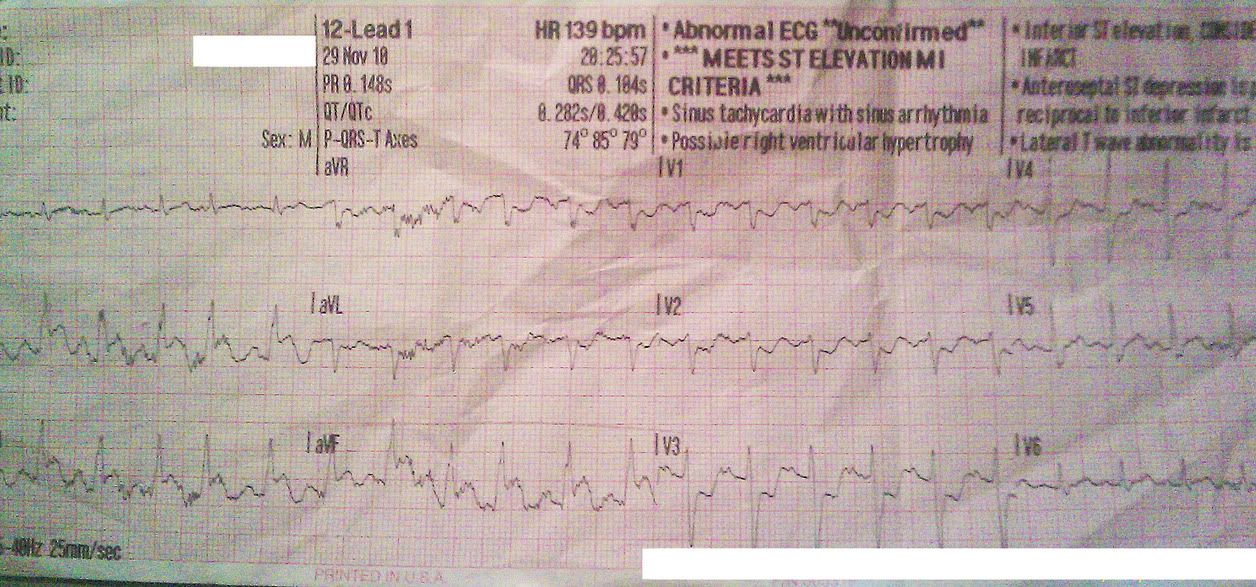
Typical inferior MI right? So we gave the pt ASA and took off for the closest hospital with a cath lab. After 8 or so tries we are still unable to get a BP, so no nitro. We gave 50mcg of Fentanyl for pain. After 5 minutes the patient was drastically less physically agitated, and became very lethargic. No change in vitals.
At the hospital the ER doc spent about 2 minutes with him and then confirmed the cath lab activation. They got a pulse in the 130s, with a BP of 55/47. They gave him heparin, plavix, fluids, dopamine etc and whisked him off to the cath lab.
On the way there they decided to stop at CT and grab a quick scan. Which was probably a good thing, since it showed the dissecting AAA the pt ALSO had going on.
The last thing I heard he had been shipped to the bigger hospital, and was in surgery with a pulse. When he arrived at that hospital he had fluids and blood running and a BP of 60/crap. I'm hoping to find out tonight if he lived through the sugery.
Arrive on scene and find an adult male lying on the living room floor, alive, writhing around. The ALS fire crew is attempting to assess the patient. The pt is a late 60's male who had been outside for less than 5 minutes doing physical labor. He had a witnessed collapse and was reported to be unresponsive for 1-2 minutes, before waking up and being moved back into the house. The only thing the family can tell us is that he takes nitro, and he has been complaining of back pain today, which he attributed to a pulled muscle.
The 3 lead is showing sinus tach at 144, resps of 28, the NIBP is showing error, we can't hear anything and he has no radial pulse. The SpO2 is 86% on 12 lpm. The pt is pale/grey and diaphoretic. His distal cap refill is slow, and his hands are cold. He looks bad.
In order to obtain an IV and 12 lead the patient has to be manually restrained because he will not hold still and doesn't even appear to hear you asking him to follow directions. The only thing he will say is that his chest hurts and he needs to move.
12 lead showed the following. Sorry, it is a crappy copy of a crappy tracing, but it shows enough to get the point.
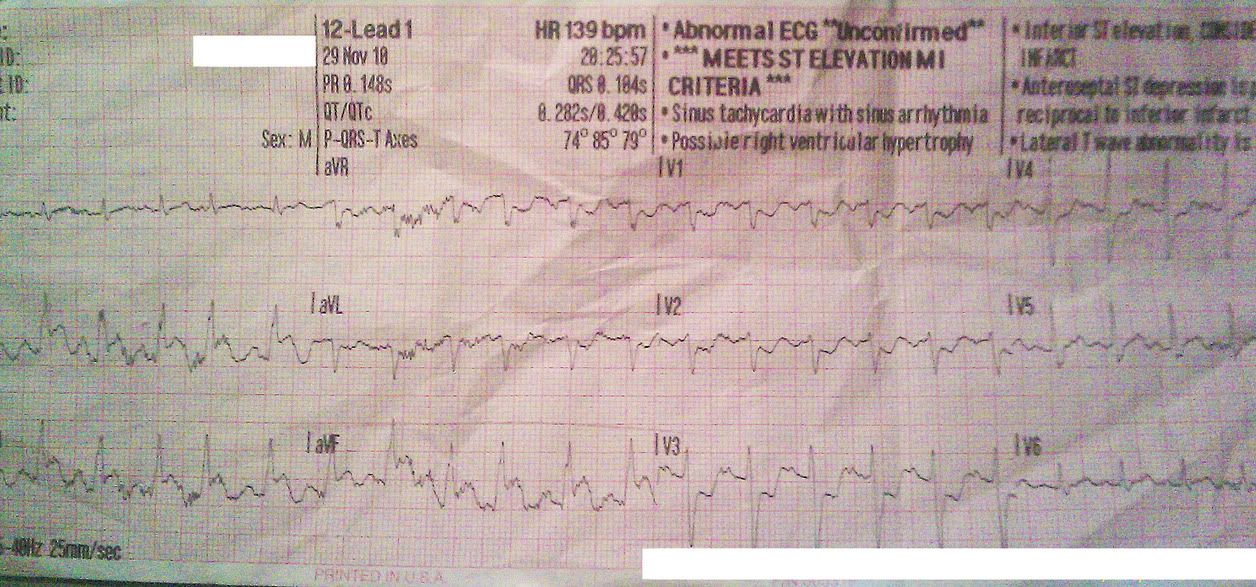
Typical inferior MI right? So we gave the pt ASA and took off for the closest hospital with a cath lab. After 8 or so tries we are still unable to get a BP, so no nitro. We gave 50mcg of Fentanyl for pain. After 5 minutes the patient was drastically less physically agitated, and became very lethargic. No change in vitals.
At the hospital the ER doc spent about 2 minutes with him and then confirmed the cath lab activation. They got a pulse in the 130s, with a BP of 55/47. They gave him heparin, plavix, fluids, dopamine etc and whisked him off to the cath lab.
On the way there they decided to stop at CT and grab a quick scan. Which was probably a good thing, since it showed the dissecting AAA the pt ALSO had going on.
The last thing I heard he had been shipped to the bigger hospital, and was in surgery with a pulse. When he arrived at that hospital he had fluids and blood running and a BP of 60/crap. I'm hoping to find out tonight if he lived through the sugery.
