This is a 12 lead from a post narrow complex PEA cardiac arrest. History of dementia and type II diabetes. No recent illness, husband states 20 min earlier, the patient had requested assistance to the washroom where she collapsed off the toilet. Fire department arrived first, and state they palpated a weak bradycardic carotid. On EMS arrival, the patient was in a bradycardic PEA. ROSC was established following 3 doses of 1mg Epi Q 3, 500ml NS bolus and intubation. Following ROSC patient was in a bradycardic sinus bradycardia and treated with nondemand transcutaneous pacing at 110mA at a rate of 70. Pulses were subsequently lost approximately 10 min after TCP was initiated. TCP was discontinued and the patient received another round of CPR and 1 dose of EPI, which resulted in ROSC (this time not bradycardic). Once extricated and in the ambulance I noted a wide complex tachycardia running across my monitor, the patient did have a pulse with this rhythm. I opted not to touch it and transport to the hospital.
My question for everyone is, do you think this is a SVT with LBB, VT, massive STEMI or hyperkalemia??
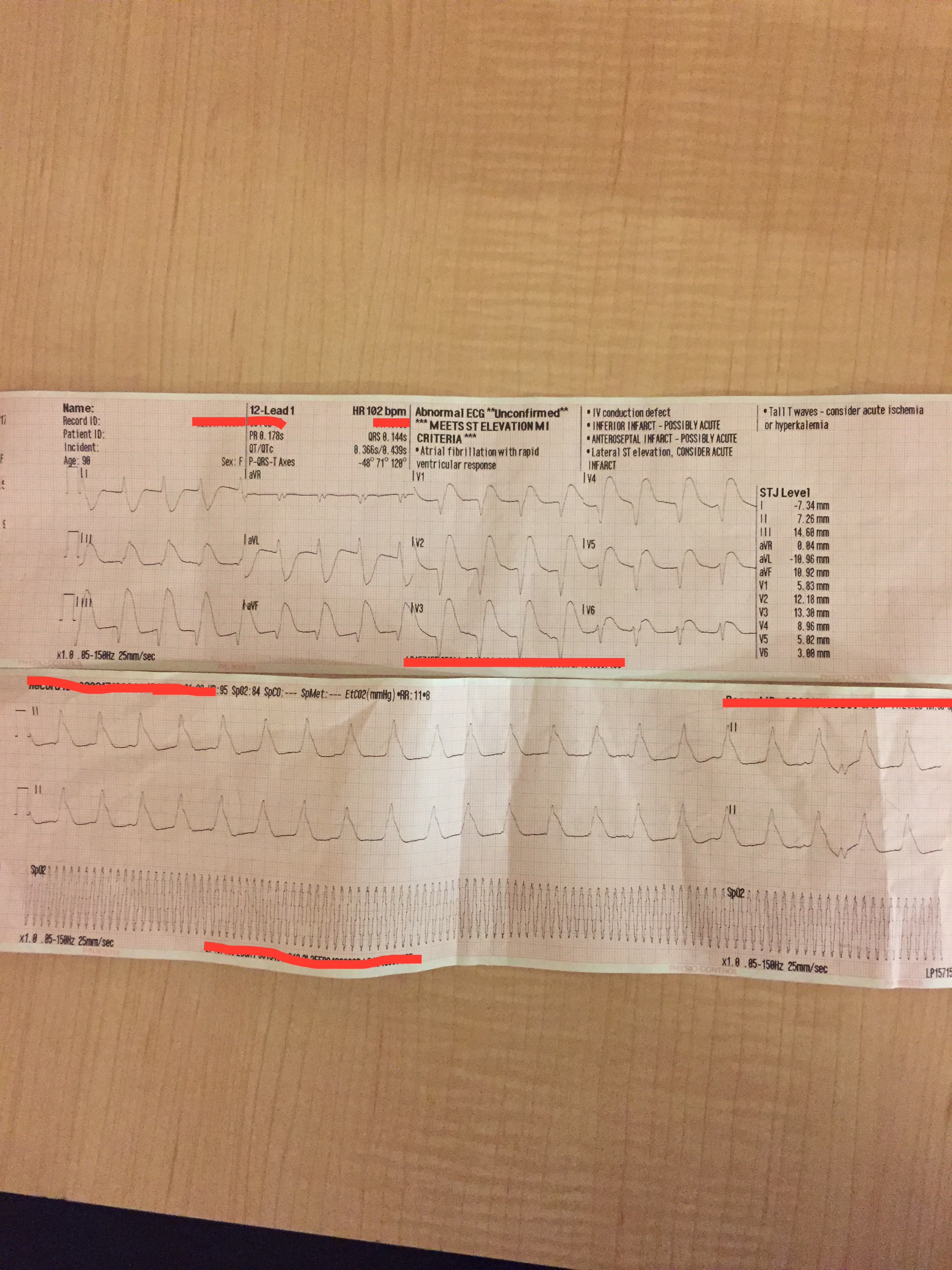
My question for everyone is, do you think this is a SVT with LBB, VT, massive STEMI or hyperkalemia??
Last edited:
