kindofafireguy
Forum Crew Member
- 97
- 1
- 6
I couldn't find this exact question anywhere, but if it's already answered somewhere please forgive me.
Had this question on my paramedic homework:
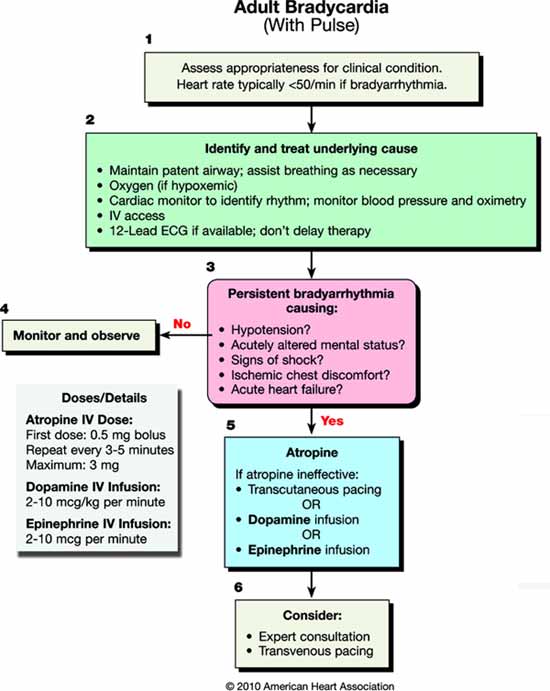
. Your patient is in sinus bradycardia at a rate of 36 beats per minute when you arrive. She relates that she has been feeling weak and dizzy but otherwise seems fine. You determine to start an IV and administer 0.5 mg of atropine. Immediately after administration, your patient’s heart rate drops to 16 beats per minute and she loses consciousness.
a. what mistake did you must likely make?
b. what should you do to correct the situation?
I'm assuming it's a reflex bradycardia of some sort but I'm confused on the action. If it's obvious, I'm going to beat myself.
Had this question on my paramedic homework:
. Your patient is in sinus bradycardia at a rate of 36 beats per minute when you arrive. She relates that she has been feeling weak and dizzy but otherwise seems fine. You determine to start an IV and administer 0.5 mg of atropine. Immediately after administration, your patient’s heart rate drops to 16 beats per minute and she loses consciousness.
a. what mistake did you must likely make?
b. what should you do to correct the situation?
I'm assuming it's a reflex bradycardia of some sort but I'm confused on the action. If it's obvious, I'm going to beat myself.