captaindepth
Forum Lieutenant
- 151
- 60
- 28
You are dispatched for a 60-70y/o male pt with chest pain @ 0630
U/A Pt was pale/cool/ and extremely diaphoretic. Pt appeared lethargic but alert and able to answer questions appropriately. BP unobtainable (manual attempt x 2), no distal pulses, and a RR of 20. The wife sates he had been awake for approx 30minutes before he had sudden weakness and shortness of breath.
You are in an urban system with about a 15 minute transport to a Level I trauma center with all services available.
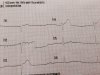
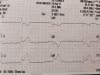
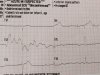
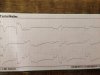
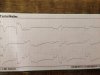
Here is the initial 4 lead EKG obtained in the house:
What are your treatment priorities? Any pharmacological interventions you would consider? How long should the on scene time be? and how would you transport the pt, emergent vs. nonemergent?
U/A Pt was pale/cool/ and extremely diaphoretic. Pt appeared lethargic but alert and able to answer questions appropriately. BP unobtainable (manual attempt x 2), no distal pulses, and a RR of 20. The wife sates he had been awake for approx 30minutes before he had sudden weakness and shortness of breath.
You are in an urban system with about a 15 minute transport to a Level I trauma center with all services available.
Here is the initial 4 lead EKG obtained in the house:
What are your treatment priorities? Any pharmacological interventions you would consider? How long should the on scene time be? and how would you transport the pt, emergent vs. nonemergent?