Quick question on this. Are pacemakers always supposed to show a spike right before the P wave (acting as SA)? Or do they spike at various points (or does that just mean they're malfunctioning

)
Would something like a neurostimulator, or any distal stimulator, be able to show a spike on a 12 lead..?
1. Are pacemakers always supposed to show a spike right before the P-wave (acting as SA)?
If the pacemaker has an atrial pacing lead, then yes it can show the spike just prior to the P-wave. In this instance it would be acting in lieu of the SA node (or supplementing the SA node).
The "mode" of a pacemaker can be determined by its 3 letter code (NASPE code/NBG code, may have more letters), such as VOO, VVI, DDD, AAI, etc.
The first letter is the chamber(s) being paced: A = atria, V = ventricle, D = both atria and ventricle can be paced.
The second letter is the chamber(s) being sensed: A = atria, V = ventricle, D = both atria and ventricles can be sensed, O = no sensing.
The third letter is the response to sensed impulses: O = no response, I = inhibit pacing, T = triggered pacing, D = inhibition and triggering.
A paramedic who paces a patient using their monitor in fixed mode is doing VOO pacing. V = pacing the ventricles, O = no sensing, O = no response.
A paramedic who paces a patient using their monitor in demand mode is doing VVI pacing. V = pacing the ventricles, V = sensing the ventricles, I = do not pace if it senses the patient's own ventricular impulses.
A patient with an atrial pacemaker could have an AAI setup to, (A) pace the atria, (A) sense for normal atrial beats, (I) and do not pace if the patient's own P-waves are working.
An extremely common pacemaker setting is "DDD", which means (D) pace the atria and/or the ventricles, (D) watching both for normal activity, (D) don't pace a chamber if it is working but pace a chamber that "falls behind".
2. ...or do they spike at various points?
This depends on what pacing leads are present. An atrial lead should pace just prior to the P-wave. A ventricular lead should pace just prior to the QRS complex. Patients with biventricular pacing will have 2 pacing spikes for their QRS in close succession. Usually one just before the QRS and one ~20ms later during the QRS.
3. ...or does that just mean they're malfunctioning?
Sometimes you can determine if the leads are misplaced or if the sensing threshold is too low, or other problems with pacemakers based on what you see it doing. If you do not know the mode of operation, you can make educated guesses based on its behavior.
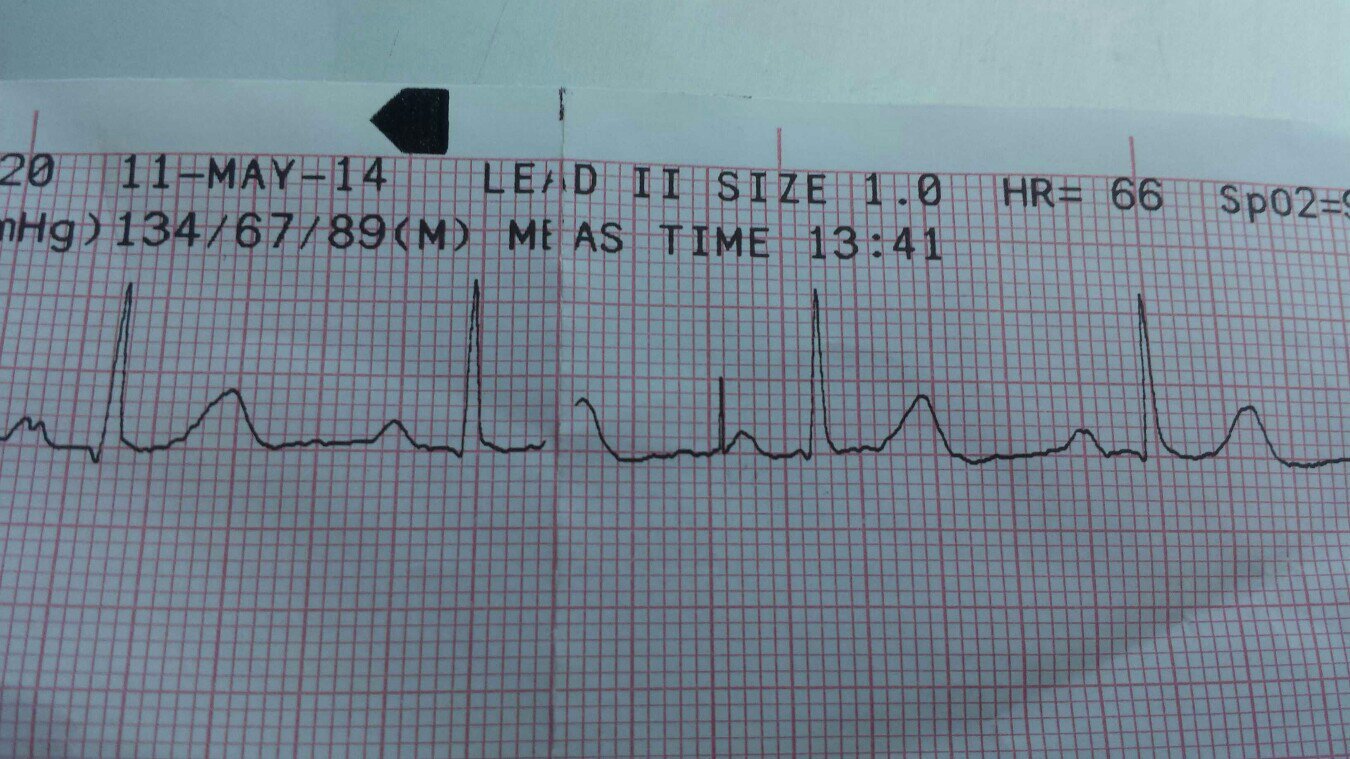
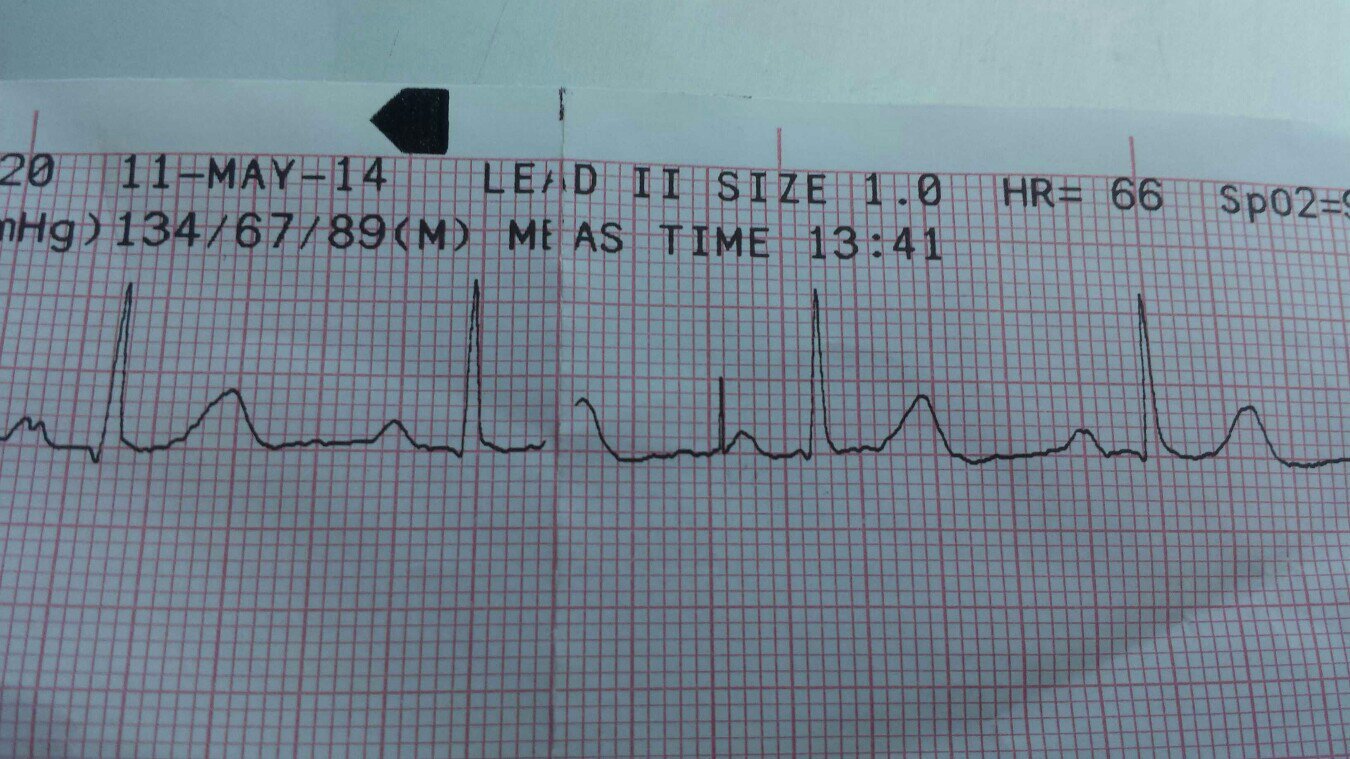
In this case, we have a lone "paced" P-wave (I'm using quotes because I don't believe it is) which is 920 ms after the prior P-wave. If this were atrial pacing, it would mean the "lower rate limit" is set to 65 bpm.
Sometimes you'll see spurious pacing spikes in patients with pacemakers which may not indicate a problem. If the timing is just right the patient's own heart may fire at nearly the same time the pacemaker fires, however, typically the pacemaker will notice this and stop pacing.
Pacemakers are wonderfully complex devices, with custom programming to handle a wide range of scenarios. Many include rate modulation to ensure the atrial or ventricular rate meets the cardiovascular demands of the patient!
4. Would something like a neurostimulator, or any distal stimulator, be able to show a spike on a 12 lead..?
Yep, this sort of artifact is commonly seen on 12-Lead ECG's due to the filter settings. In monitoring mode it may not be visible.