Smellypaddler
Forum Probie
- 27
- 4
- 3
Wondering if anyone can explain the patho related to a pt I transported today who had decorticate type posturing with a high GCS.
Pt was a 70yoM transfer out of a regional hospital who initially presented with sudden onset neck pain and bilateral arm pain. On arrival of the pt was agitated due to pain, had recently had 2.5mg IV Morphine and pinpoint pupils (initially considered to be opioid related). He had a GCS of 14 (E3, V5, M6) and was able to move all 4 limbs, nil grip strength and was holding his arms in a slightly flexed manner similar to the onset of decorticate posturing. Handover at the hospital was that the pt had an unknown mass at C4 ?haematoma, tumor or abcess.
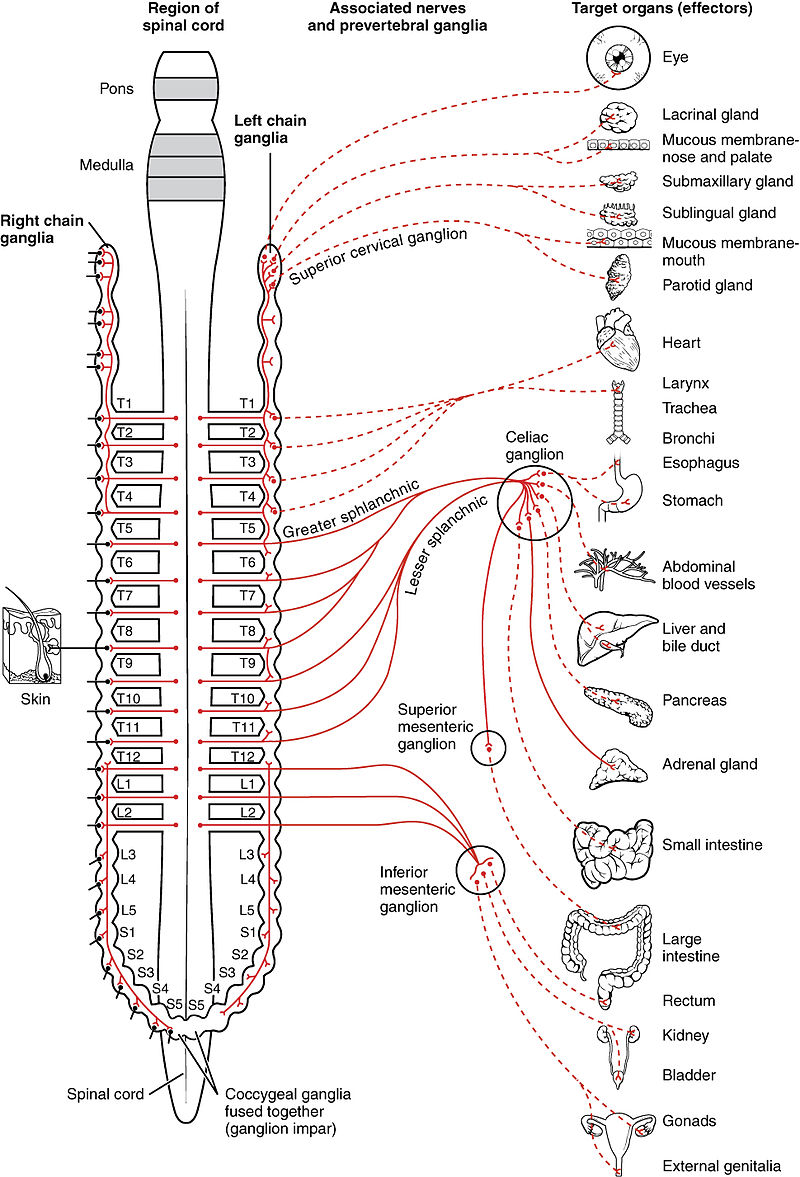
Pt given 25mcg IV Fentanyl, pt became drowsy yet easily rouseable with well controlled pain. During the 2.5hr transport the pt progressively deteriorated becoming hypotensive, bradycardic with increased decorticate type posturing. By arrival at hospital they had nil sensation or movement from below the sternum, nil sensation and uncontrolled movement of upper limbs and decorticate posturing, pinpoint pupils remained despite nil further opiates and paradoxical breathing. Pt dropped HR to 35bpm, Systolic BP to 75 and required atropine.
Despite all of their symptoms the pt remained GCS 14 throughout.
Everything I could think of involved brain stem herniation with possible pontine involvement but I am at a loss to explain the posturing with such a high GCS.
Any ideas?
Pt was a 70yoM transfer out of a regional hospital who initially presented with sudden onset neck pain and bilateral arm pain. On arrival of the pt was agitated due to pain, had recently had 2.5mg IV Morphine and pinpoint pupils (initially considered to be opioid related). He had a GCS of 14 (E3, V5, M6) and was able to move all 4 limbs, nil grip strength and was holding his arms in a slightly flexed manner similar to the onset of decorticate posturing. Handover at the hospital was that the pt had an unknown mass at C4 ?haematoma, tumor or abcess.
Pt given 25mcg IV Fentanyl, pt became drowsy yet easily rouseable with well controlled pain. During the 2.5hr transport the pt progressively deteriorated becoming hypotensive, bradycardic with increased decorticate type posturing. By arrival at hospital they had nil sensation or movement from below the sternum, nil sensation and uncontrolled movement of upper limbs and decorticate posturing, pinpoint pupils remained despite nil further opiates and paradoxical breathing. Pt dropped HR to 35bpm, Systolic BP to 75 and required atropine.
Despite all of their symptoms the pt remained GCS 14 throughout.
Everything I could think of involved brain stem herniation with possible pontine involvement but I am at a loss to explain the posturing with such a high GCS.
Any ideas?