Grady_emt
Forum Captain
- 301
- 0
- 0
Just looking to see what you guys think this rhythm (esp the initial one) is. I havent a clue, and we got totally different answers from each doc we asked.:unsure:
So on the last night of a long weekend, approx 0345 hrs my partner and I were dispatched to a Code 1 "Diff Breathing, Severe Resp. Distress/Cardiac Hx" with a BLS engine (we are ALS). Upon arrival, 54 yof pt found lying on left side in bed, and looks like crap (note, we have run this pt several times, normally very talkative and alert) Hx: Acute Renal Failure/Dialysis Pt, Diabetic, HTN, ^cholesterol, MI in 2001. Per roomate, pt is M/W/F Dialysis pt and last went on F of last week, and has been non-compliant with any of her meds x 3 weeks, which are the usual dialysis pt full-grocery-bag variety.
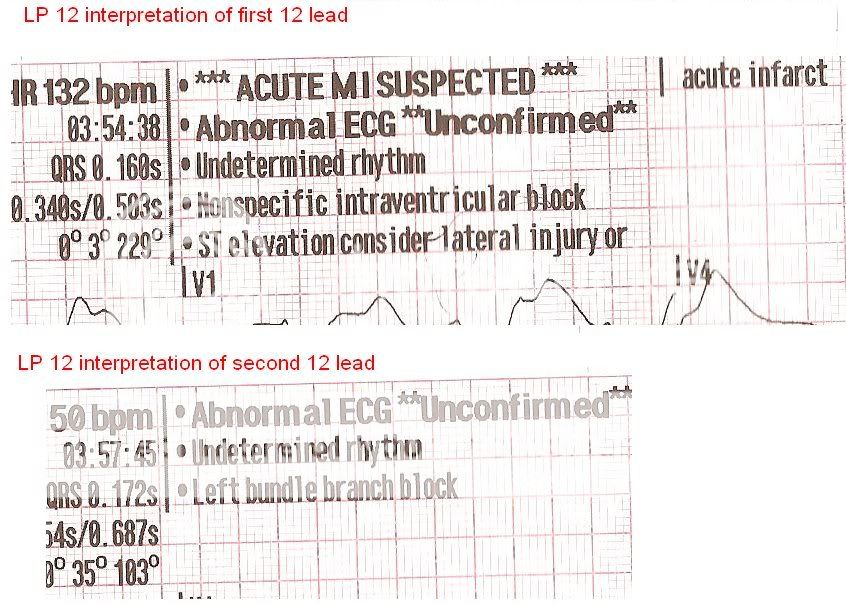
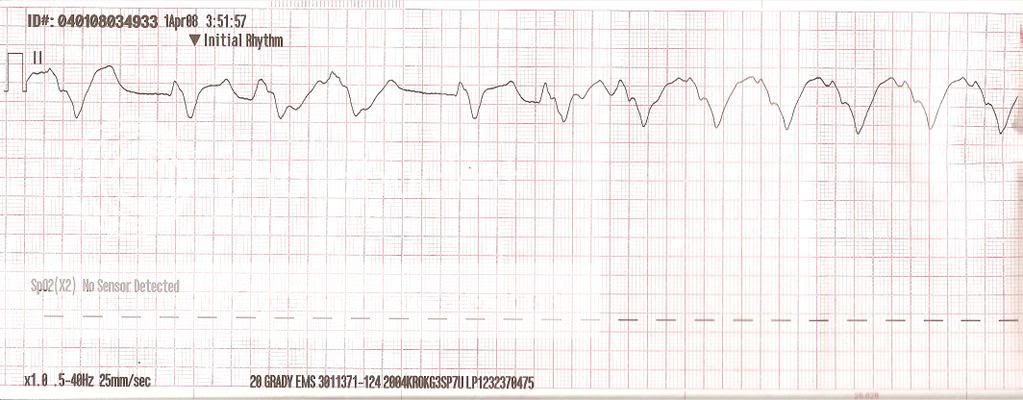
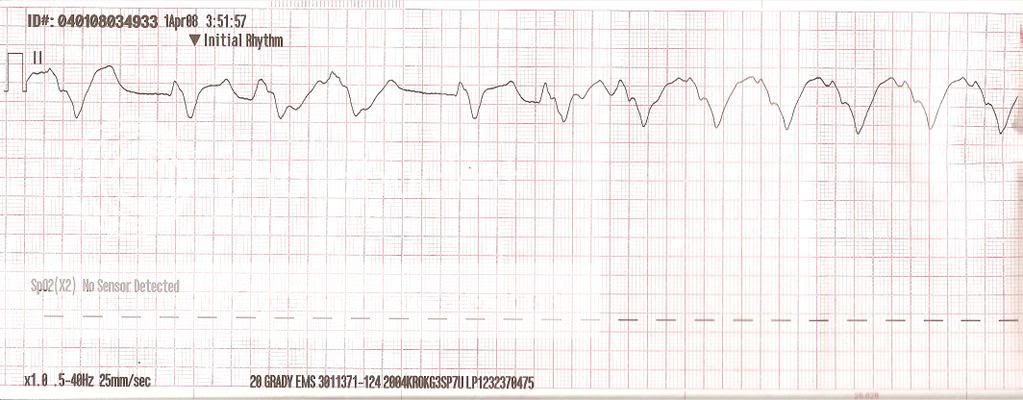
She looks like crap, resp approx 34-26, pulse 46 and thready, pressure 136/80, pulse ox 84 on room air. While awaiting fire for extrication assist from 2nd flr, pt placed on NRB, and the monitor was applied to show this...
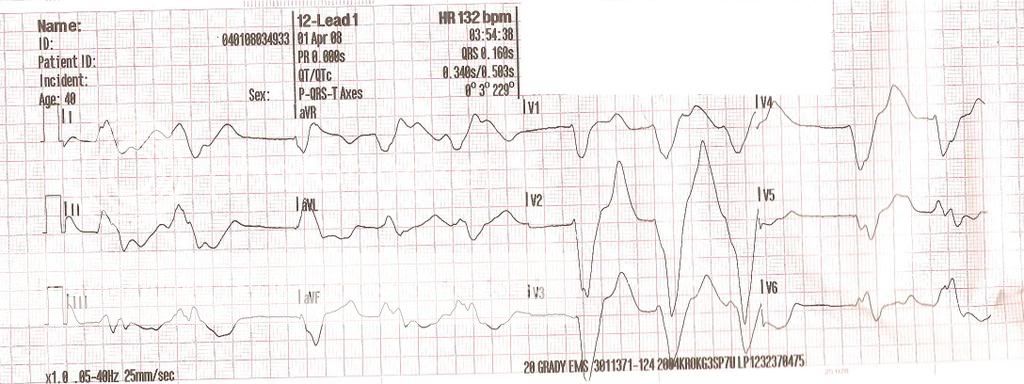
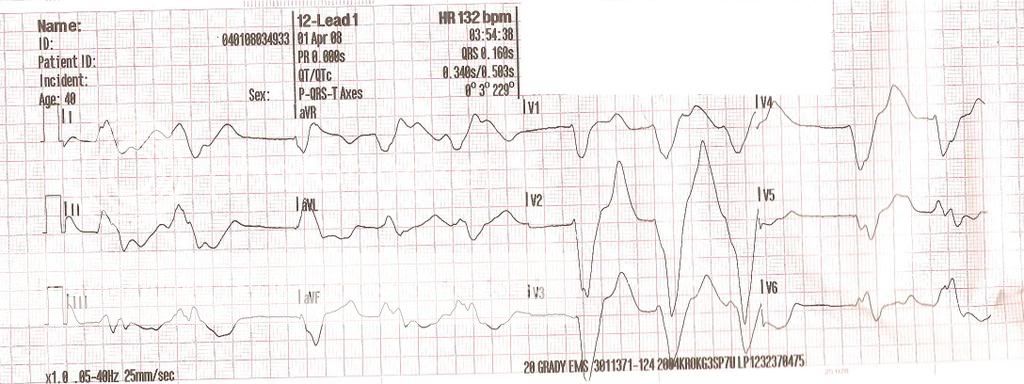
Pt is non verbal except "need some oxygen" over about 6 breaths. extricated to unit, 12 lead applied to show
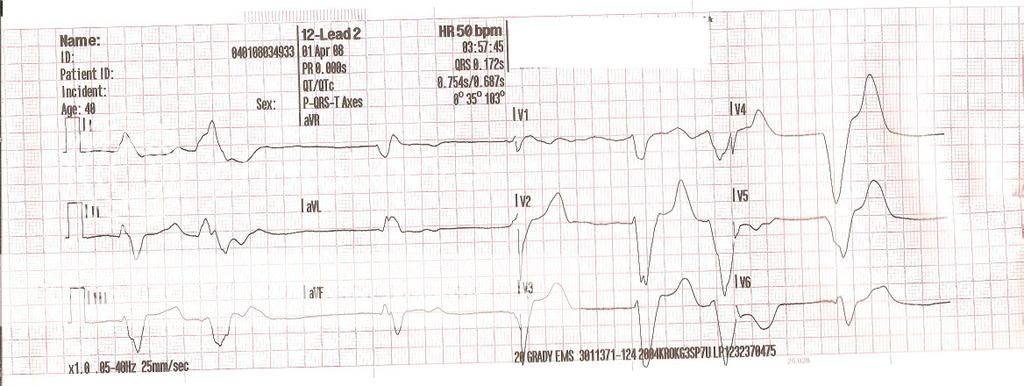
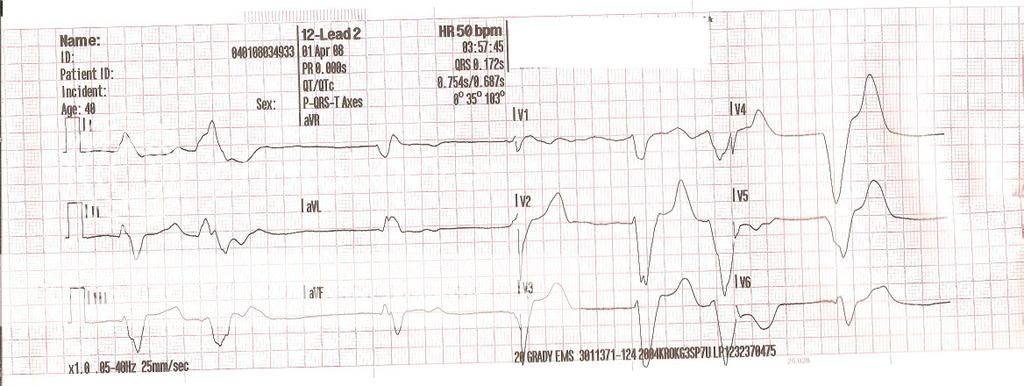
Breath sounds are clear, - edema noted, pale mucosa, poor skin turgor, unable to establish IV (everythings all scarred over, EJ is completely flat). One more 12lead before leaving scene shows
We had about a 5 minute transport to ER, where pt went into v-fib that was defib-ed into Torsades, that after 4g MagSulf, 2xBiCarb, 2xEpi, 2xAtro, Calcium Gluconate, and Calcium Chloride, and D50, pt was again defib-ed into a sinus-ish rhythm with a pulse that she maintained for about 10 minutes before degrading back to v-fib which became her terminal rhythm.:wacko:
So on the last night of a long weekend, approx 0345 hrs my partner and I were dispatched to a Code 1 "Diff Breathing, Severe Resp. Distress/Cardiac Hx" with a BLS engine (we are ALS). Upon arrival, 54 yof pt found lying on left side in bed, and looks like crap (note, we have run this pt several times, normally very talkative and alert) Hx: Acute Renal Failure/Dialysis Pt, Diabetic, HTN, ^cholesterol, MI in 2001. Per roomate, pt is M/W/F Dialysis pt and last went on F of last week, and has been non-compliant with any of her meds x 3 weeks, which are the usual dialysis pt full-grocery-bag variety.
She looks like crap, resp approx 34-26, pulse 46 and thready, pressure 136/80, pulse ox 84 on room air. While awaiting fire for extrication assist from 2nd flr, pt placed on NRB, and the monitor was applied to show this...
Pt is non verbal except "need some oxygen" over about 6 breaths. extricated to unit, 12 lead applied to show
Breath sounds are clear, - edema noted, pale mucosa, poor skin turgor, unable to establish IV (everythings all scarred over, EJ is completely flat). One more 12lead before leaving scene shows
We had about a 5 minute transport to ER, where pt went into v-fib that was defib-ed into Torsades, that after 4g MagSulf, 2xBiCarb, 2xEpi, 2xAtro, Calcium Gluconate, and Calcium Chloride, and D50, pt was again defib-ed into a sinus-ish rhythm with a pulse that she maintained for about 10 minutes before degrading back to v-fib which became her terminal rhythm.:wacko: