I know it's been a few months, but a recent case deserved a posting.
CCT unit, dispatched at 0200 for a transfer from a smallish ICU to Big City Medical Center 20 minutes away. The only info you've got is the patient is "trached and on drips".
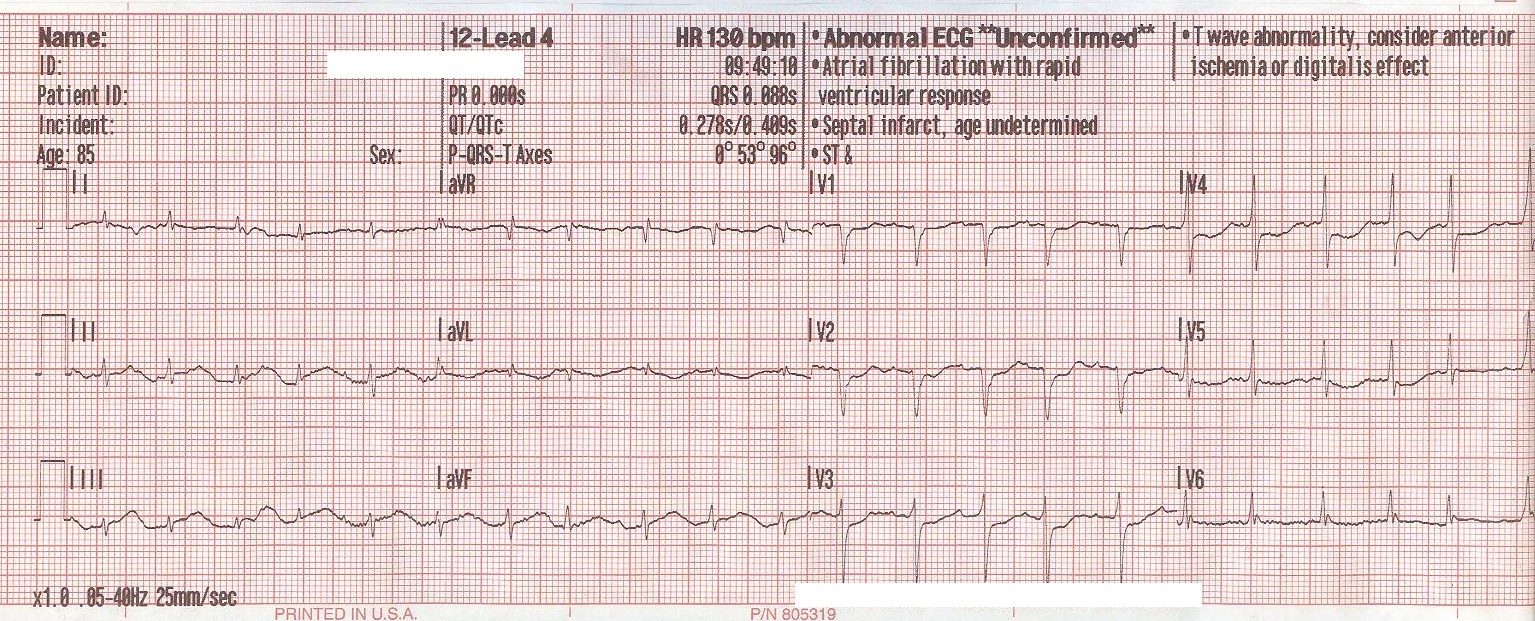
On arrival you find a crowd of people with a "deer in the head lights" look standing at bedside of a 46 YOF three hours post-ROSC. The patient was 10 days post-CABG, had been extubated and was scheduled to go home the next day when she suffered a hyperkalemic arrest and required CPR, multiple defibrilations, calcium, bicarb, insulin and D50. The patient had multiple failed airway attempts and had been crich'ed with a 6.0 ETT. You see Levophed and Dopamine hanging, the nurse is telling you she's turning the midazolam drip off now that your here.
The physician is at bedside telling you to "hurry up and get the hell out of here!"
Go....
CCT unit, dispatched at 0200 for a transfer from a smallish ICU to Big City Medical Center 20 minutes away. The only info you've got is the patient is "trached and on drips".
On arrival you find a crowd of people with a "deer in the head lights" look standing at bedside of a 46 YOF three hours post-ROSC. The patient was 10 days post-CABG, had been extubated and was scheduled to go home the next day when she suffered a hyperkalemic arrest and required CPR, multiple defibrilations, calcium, bicarb, insulin and D50. The patient had multiple failed airway attempts and had been crich'ed with a 6.0 ETT. You see Levophed and Dopamine hanging, the nurse is telling you she's turning the midazolam drip off now that your here.
The physician is at bedside telling you to "hurry up and get the hell out of here!"
Go....