Navigation
Install the app
How to install the app on iOS
Follow along with the video below to see how to install our site as a web app on your home screen.
Note: This feature may not be available in some browsers.
More options
Style variation
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
the 100% directionless thread
- Thread starter KEVD18
- Start date
teedubbyaw
Forum Deputy Chief
- 1,036
- 461
- 83
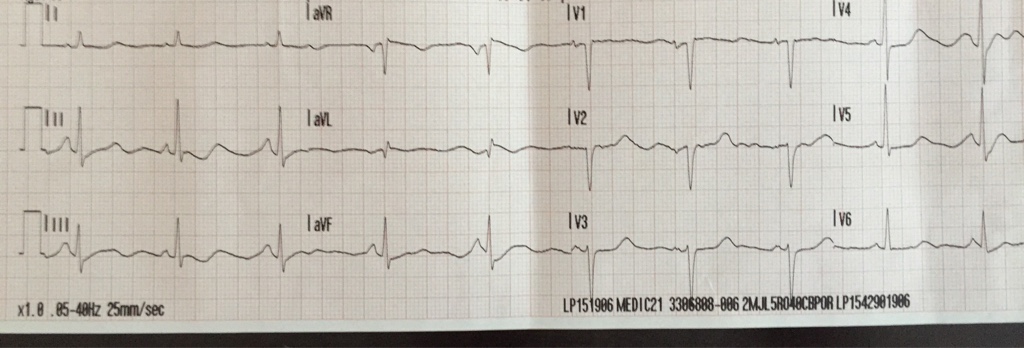
Interp!
- 2,735
- 1,272
- 113
Lown-Ganong-Levine
Jim37F
Forum Deputy Chief
- 4,387
- 3,032
- 113
So I filled out a paper PCR today for the first time in a year
No clinical vignette? A cold read? :[
62, normal sinus rhythm, possibly prolonged QT, artifacts.
Rate:62
Rhythm: Regularly regular narrow complex rhythm. P-waves present and associated with complexes. PRi is less than 0.2s, but probably still around 0.12-0.16 looking at lead II. No delta waves appreciated. Normal sinus rhythm.
Existence of LGL has been questioned. Short PRi can be due to foci originating in atria or junction. It could be due to the patient being a pediatric, but there aren't other signs of this being a pediatric in this ECG (faster heart rate, T-wave inversion in V1-3, right axis deviation, pseudo-RBBB pattern).
The QTc looks long in lead V6. If you said the rate was 60, the QTc would probably be around 520-560 ms! Due to artifact? U-wave? Congenital prolonged QT? Electrolyte imbalance? Drugs?
Frontal QRS axis near +60 degrees due to aVL being the smallest and biphasic. Normal!
Transverse QRS axis near +40 degree due to lead V4 being the point of transition. Normal! V3 has a pretty short R-wave. Probably misplaced.
Sometimes the P-wave looks tall, but it looks more like artifact to me than anything. There are mild artifact throughout this ECG. I don't believe there are signs of hypertrophy or enlargement on this ECG.
Insignificant q-wave in aVL. No other appreciated q-waves or ST/T changes.
To be honest, I would be looking at the ECG's number to see what it got. It does look like mild artifacts throughout so I would like a repeat. If this patient got an ECG due to suspected ACS then I would be doing a repeat ECG q15 minutes, with vitals, change in patient's condition, etc.
For the most part, I wouldn't have found this ECG interesting.
62, normal sinus rhythm, possibly prolonged QT, artifacts.
Rate:62
Rhythm: Regularly regular narrow complex rhythm. P-waves present and associated with complexes. PRi is less than 0.2s, but probably still around 0.12-0.16 looking at lead II. No delta waves appreciated. Normal sinus rhythm.
Existence of LGL has been questioned. Short PRi can be due to foci originating in atria or junction. It could be due to the patient being a pediatric, but there aren't other signs of this being a pediatric in this ECG (faster heart rate, T-wave inversion in V1-3, right axis deviation, pseudo-RBBB pattern).
The QTc looks long in lead V6. If you said the rate was 60, the QTc would probably be around 520-560 ms! Due to artifact? U-wave? Congenital prolonged QT? Electrolyte imbalance? Drugs?
Frontal QRS axis near +60 degrees due to aVL being the smallest and biphasic. Normal!
Transverse QRS axis near +40 degree due to lead V4 being the point of transition. Normal! V3 has a pretty short R-wave. Probably misplaced.
Sometimes the P-wave looks tall, but it looks more like artifact to me than anything. There are mild artifact throughout this ECG. I don't believe there are signs of hypertrophy or enlargement on this ECG.
Insignificant q-wave in aVL. No other appreciated q-waves or ST/T changes.
To be honest, I would be looking at the ECG's number to see what it got. It does look like mild artifacts throughout so I would like a repeat. If this patient got an ECG due to suspected ACS then I would be doing a repeat ECG q15 minutes, with vitals, change in patient's condition, etc.
For the most part, I wouldn't have found this ECG interesting.
teedubbyaw
Forum Deputy Chief
- 1,036
- 461
- 83
60's F with presumed cardiac arrest, witnessed, cpr and AED used. Pulses present on scene, but she presented with what I interpreted as Afib w/ rvr (rates as high as 190), pvc's. Cardioverted w/ slight rate decrease. Conversion to nsr in the 60's during intubation. I'll post pics of initial rhythm in the morning. Healthy looking lady. Interesting call. She wound up in the cath lab with a stent placed.
I had something similar. I had a 70 y/o Male in a SNF in cardiac arrest during my internship. Initially asystole. Did CPR and 2-3 mg epi I think. He went into a PEA idioventricular rhythm and then normal sinus rhythm with ROSC. I thought it was really interesting how you couldn't really tell that the patient had just been in cardiac arrest.60's F with presumed cardiac arrest, witnessed, cpr and AED used. Pulses present on scene, but she presented with what I interpreted as Afib w/ rvr (rates as high as 190), pvc's. Cardioverted w/ slight rate decrease. Conversion to nsr in the 60's during intubation. I'll post pics of initial rhythm in the morning. Healthy looking lady. Interesting call. She wound up in the cath lab with a stent placed.
After my post, I thought the QTc thing might be a bit absurd. I kinda felt like it was probably more likely artifact or just not being able to see well. People seem to uncomfortable with calling an ECG normal. Perhaps I wasn't wrong about it and that it was a sign of ischemia.
COmedic17
Forum Asst. Chief
- 912
- 638
- 93
Well, I'll point out the things that aren't normal...
1) Tachycardia (#1 ECG sign with pulmonary embolism)
2) Right axis deviation (lead I is negative, II, III and aVF are positive). Could be due to a pulmonary disease like a pulmonary embolism or something chronic. This is pretty extreme though and there aren't signs of right ventricular hypertrophy in the precordial leads (taller R-wave in the anteroseptal leads with the R-wave decrease as the leads become more lateral and negative T-waves in the anteroseptal leads V1-4). This makes me suspicious of right arm and left arm lead reversal.
The ECG says possible left posterior fascicular block (LPFB), which usually is just shown as right axis deviation and you have ruled out other causes of right axis deviation. Isolated LPFB is extremely rare. It's way more common to see it in a bifascicular (RBBB + LPFB) or trifascicular block (RBBB + LPFB + 1st degree AVB). I doubt this is LPFB.
Occam's razor. Probably right arm and left arm lead reversal.
3) Again, lead V3 has a small R wave. I am wondering if both previous ECGs have weird V3 because the patients were female, lol. The machine says it is a 24 y/o Female. Never thought about it before. We should call it the V3 sign or something.
4) Looks like lead III has a qR wave with a negative T-wave. Some people talk about S1Q3T3 sign with pulmonary embolism. This sign is actually associated with right ventricular hypertrophy.
Without a clinical vignette, I am not certain if this is due to a pulmonary embolism, but it is possible. Any recent surgery? Recent trauma? Recent long distance trip or any reason she wouldn't move a lot? Birth controls also increase her chance of having a pulmonary embolism. If she smokes, her odds of pulmonary embolism is higher.
So my guesses are pulmonary embolism (or other pulmonary disease) or right arm and left arm lead reversal with tachycardia secondary to something else.
1) Tachycardia (#1 ECG sign with pulmonary embolism)
2) Right axis deviation (lead I is negative, II, III and aVF are positive). Could be due to a pulmonary disease like a pulmonary embolism or something chronic. This is pretty extreme though and there aren't signs of right ventricular hypertrophy in the precordial leads (taller R-wave in the anteroseptal leads with the R-wave decrease as the leads become more lateral and negative T-waves in the anteroseptal leads V1-4). This makes me suspicious of right arm and left arm lead reversal.
The ECG says possible left posterior fascicular block (LPFB), which usually is just shown as right axis deviation and you have ruled out other causes of right axis deviation. Isolated LPFB is extremely rare. It's way more common to see it in a bifascicular (RBBB + LPFB) or trifascicular block (RBBB + LPFB + 1st degree AVB). I doubt this is LPFB.
Occam's razor. Probably right arm and left arm lead reversal.
3) Again, lead V3 has a small R wave. I am wondering if both previous ECGs have weird V3 because the patients were female, lol. The machine says it is a 24 y/o Female. Never thought about it before. We should call it the V3 sign or something.
4) Looks like lead III has a qR wave with a negative T-wave. Some people talk about S1Q3T3 sign with pulmonary embolism. This sign is actually associated with right ventricular hypertrophy.
Without a clinical vignette, I am not certain if this is due to a pulmonary embolism, but it is possible. Any recent surgery? Recent trauma? Recent long distance trip or any reason she wouldn't move a lot? Birth controls also increase her chance of having a pulmonary embolism. If she smokes, her odds of pulmonary embolism is higher.
So my guesses are pulmonary embolism (or other pulmonary disease) or right arm and left arm lead reversal with tachycardia secondary to something else.
Last edited:
COmedic17
Forum Asst. Chief
- 912
- 638
- 93
All leads were correctly placed.Well, I'll point out the things that aren't normal...
1) Tachycardia (#1 ECG sign with pulmonary embolism)
2) Right axis deviation (lead I is negative, II, III and aVF are positive). Could be due to a pulmonary disease like a pulmonary embolism or something chronic. This is pretty extreme though and there aren't signs of right ventricular hypertrophy in the precordial leads (taller R-wave in the anteroseptal leads with the R-wave decrease as the leads become more lateral and negative T-waves in the anteroseptal leads V1-4). This makes me suspicious of right arm and left arm lead reversal.
The ECG says possible left posterior fascicular block (LPFB), which usually is just shown as right axis deviation and you have ruled out other causes of right axis deviation. Isolated LPFB is extremely rare. It's way more common to see it in a bifascicular (RBBB + LPFB) or trifascicular block (RBBB + LPFB + 1st degree AVB). I doubt this is LPFB.
Occam's razor. Probably right arm and left arm lead reversal.
3) Again, lead V3 has a small R wave. I am wondering if both previous ECGs have weird V3 because the patients were female, lol. The machine says it is a 24 y/o Female. Never thought about it before. We should call it the V3 sign or something.
4) Looks like lead III has a qR wave with a negative T-wave. Some people talk about S1Q3T3 sign with pulmonary embolism. This sign is actually associated with right ventricular hypertrophy.
Without a clinical vignette, I am not certain if this is due to a pulmonary embolism, but it is possible. Any recent surgery? Recent trauma? Recent long distance trip or any reason she wouldn't move a lot? Birth controls also increase her chance of having a pulmonary embolism. If she smokes, her odds of pulmonary embolism is higher.
So my guesses are pulmonary embolism (or other pulmonary disease) or right arm and left arm lead reversal with tachycardia secondary to something else.
Positive for orthostatic vitals.
Hypotensive. (90's over 50s while sitting)
Takes oral BC.
No surgeries/trips.
Blood glucose of 52.
HX- hypothyroidism, AI, hyperparathyroidism, asthma.
Cap refill in extremities >10 seconds.
AI = adrenal insufficiency? Weren't you the member that said had Addison or AI? Now I'm starting to have a feeling that this is an acute AI case due to the hypotension, hypoglycemia, history of AI, and because I think you were the one that had Addison, lol. Weird that you would have had that patient today (ECG is dated 03 June 15).
COmedic17
Forum Asst. Chief
- 912
- 638
- 93
Coughing. Feels sick.
St depression in v1 and avr.
Mild elevation in other leads (nothing major)
Some diffuse pr segment depression.
Fever of 101.3
Squeaky heart sounds.
St depression in v1 and avr.
Mild elevation in other leads (nothing major)
Some diffuse pr segment depression.
Fever of 101.3
Squeaky heart sounds.
COmedic17
Forum Asst. Chief
- 912
- 638
- 93
I do have addisons. Lol.AI = adrenal insufficiency? Weren't you the member that said had Addison or AI? Now I'm starting to have a feeling that this is an acute AI case due to the hypotension, hypoglycemia, history of AI, and because I think you were the one that had Addison, lol. Weird that you would have had that patient today (ECG is dated 03 June 15).
But this isn't stemmed from an endocrine problem.
It's cardiac in nature.
COmedic17
Forum Asst. Chief
- 912
- 638
- 93
When I'll get back I'll take a pic of the hospitals EKG. There's more noticeable pr depression in theirs. But they confirmed with an ultrasound.Sounds like you are trying to describe pericarditis with the PRi depression and mild ST elevation. Coughing and feeling sick. Fever. Wouldn't have expected it from this EKG. I don't really see the ST elevation or PRi depression.
Has a wide spread autoimmune disease that attacks endocrine glands. So she had crappy immunity. has had pericarditis a couple years prior. Got sick and got it again. She knew what was wrong.
COmedic17
Forum Asst. Chief
- 912
- 638
- 93
Gurby
Forum Asst. Chief
- 818
- 597
- 93
I spy an S1Q3T3!
- 2,735
- 1,272
- 113
It's really, really hard to motivate myself to go to a 3 hour class on BLS administration of albuterol. I'm trying to help out a couple times a month by going to the nearby ambulance station and attending a call or two when they don't have anyone else available, but there are some pretty ridiculous hoops to jump through.
Evidently my state issued paramedic license doesn't allow me to attend BLS patients, so I have to go take some kind of EMT PowerPoint, learn how to administer Narcan, learn how to use CPAP, and go to this albuterol class. It's difficult to figure out how I can work on the same ambulance as a paramedic during the day and run any call I want as an ALS provider, but the moment I get off work I'm not allowed to take a manual blood pressure since I'm "not an EMT."
Beyond already being philosophically against modern volunteer EMS in most places, this really isn't encouraging me to keep trying to help out.
Evidently my state issued paramedic license doesn't allow me to attend BLS patients, so I have to go take some kind of EMT PowerPoint, learn how to administer Narcan, learn how to use CPAP, and go to this albuterol class. It's difficult to figure out how I can work on the same ambulance as a paramedic during the day and run any call I want as an ALS provider, but the moment I get off work I'm not allowed to take a manual blood pressure since I'm "not an EMT."
Beyond already being philosophically against modern volunteer EMS in most places, this really isn't encouraging me to keep trying to help out.
- 4,534
- 3,261
- 113
It's really, really hard to motivate myself to go to a 3 hour class on BLS administration of albuterol. I'm trying to help out a couple times a month by going to the nearby ambulance station and attending a call or two when they don't have anyone else available, but there are some pretty ridiculous hoops to jump through.
Exactly why my few attempts at helping out the local vollys have always been short lived.

