hellofirstresponders
Forum Crew Member
- 36
- 0
- 6
Whats the difference? Why do we not make the pt bare down, and act like their going to take a dump? Like, why won't it work on v-tach but it does on SVT?
Follow along with the video below to see how to install our site as a web app on your home screen.
Note: This feature may not be available in some browsers.
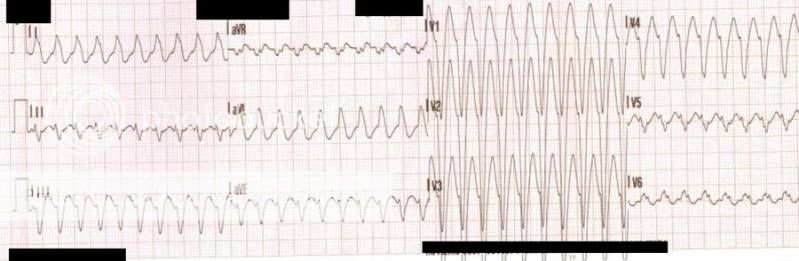
If it is VT many times they will have Extreme Right Axis Deviation ( ERAD leads I,II,III pointed down) combined with an upright V1. There are other indicators on a 12 lead that can prove VT as well.
Exactly, extreme right axis deviation, aka no mans land, and concordance in the V leads is also key to determine VTB)
The Brothers Brugada (and their cousin I think) developed a 4 step criteria (Brugada! We're not just a Syndrome anymore!) for discerning whether a rhythm is VT or SVT with aberrant conduction.
However, as TomB rightly points out, it is really largely irrelevant to a prehospital provider; any wide complex tachycardia should be considered VT and treated accordingly.
On drug therapy for VT vs. SVT...
I understand that lidocaine is a sodium channel blocker, which decreases the action potential of the myocardium, which makes it less likely impulses from the pacemaker in the ventricles will be transmitted to the myocardium to depolarize, but I don't know why this would be counterproductive in a supraventricular tachycardia, even though I know lidocaine is not indicated in these arrhythmias. I have always been taught that lidocaine suppresses the AV node, and if the patient is in a-fib or a-flutter, the hundreds of impulses per minute from the atria, now unchecked by the AV node, will likely cause the ventricles to fibrillate. This is why it is important to be able to read aberrant a-fib on the 12 lead right? Why can lidocaine cause this to happen then if its action is to inhibit the ion movement that caries the impulses responsible for myocardium depolarization? Why is this (evidently) less dangerous than a CCB for VT, and why is a CCB for VT more dangerous?
I disagree. Improper diagnosis in the field could delay the care they need.
You need to learn all steps involved. I listed one thing to check already. I check others as well and it takes me just about 3 seconds total after I take the 12 lead.
The 12 lead is 96% diagnostic for VT identification.
So patient has HR 150+. 12 lead with limb leads on limbs not torso. If any step shows VT no need to go to next step.
Step 1 ERAD(described above in my post) and upright V1
Step 2 Is lead V1 shaped as a fireman's hat, single upright steeple, or two peaks with the first taller ( big mountain little mountain )
Step 3 V1 downward and either flat R wider than 40ms or slurred or notched initial down stroke.
Step 4 V6 Any negative deflection.
Always go in order.
If not sure if VT or SVT better to use adenisone to find underlying rhythm than to kill them with lidocaine.
On drug therapy for VT vs. SVT...
I understand that lidocaine is a sodium channel blocker, which decreases the action potential of the myocardium, which makes it less likely impulses from the pacemaker in the ventricles will be transmitted to the myocardium to depolarize, but I don't know why this would be counterproductive in a supraventricular tachycardia, even though I know lidocaine is not indicated in these arrhythmias. I have always been taught that lidocaine suppresses the AV node, and if the patient is in a-fib or a-flutter, the hundreds of impulses per minute from the atria, now unchecked by the AV node, will likely cause the ventricles to fibrillate. This is why it is important to be able to read aberrant a-fib on the 12 lead right? Why can lidocaine cause this to happen then if its action is to inhibit the ion movement that caries the impulses responsible for myocardium depolarization? Why is this (evidently) less dangerous than a CCB for VT, and why is a CCB for VT more dangerous?
