Female in her 50s with acute onset of dizziness, shortness of breath and nausea. Denies chest pain, syncope vomiting or further. Only hx is hypertension and Prior MI 7 years ago. She's cool, pale diaphoretic skin signs, get into back of rig and 4 lead shows run of V-tach with pulses @ 200bpm.
Placed on pads immediately but self converts out before i can sync cardiovert. BP initially 116/72 and declines to 82/60 by er arrival (iv access and fluids already established) Lungs are clear, resp minimally labored at about 20, 12 lead comes back with the following below with acute ***STEMI*** reading.
I interperted as stemi due to Depressions in I and AVL with the noted elevations in II, III, AVF and treat as such.
Er physician stated that this isnt a stemi because there is only "notching" of the ST elevation and said something about "well who knows where her baseline REALLY is" as far as the isoelectric baseline he was refering to.
I know lead II is a bit questionalble (if any) upon further review of elevations but others definately appeared that way to me. Help me to understand where i went wrong.
Either way, its better safe than sorry and better to just do a quick code 3 transport and have it NOT be one than not treat it like that and miss it.....
but just an education moment for me! THanks guys.
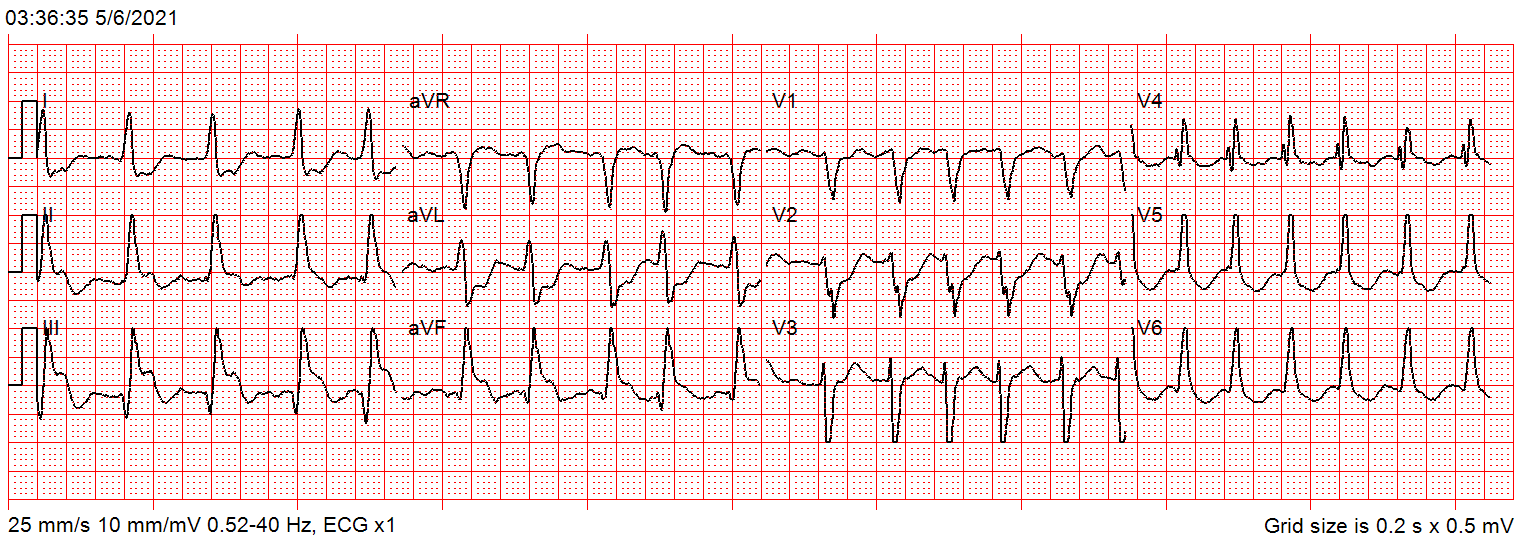
Placed on pads immediately but self converts out before i can sync cardiovert. BP initially 116/72 and declines to 82/60 by er arrival (iv access and fluids already established) Lungs are clear, resp minimally labored at about 20, 12 lead comes back with the following below with acute ***STEMI*** reading.
I interperted as stemi due to Depressions in I and AVL with the noted elevations in II, III, AVF and treat as such.
Er physician stated that this isnt a stemi because there is only "notching" of the ST elevation and said something about "well who knows where her baseline REALLY is" as far as the isoelectric baseline he was refering to.
I know lead II is a bit questionalble (if any) upon further review of elevations but others definately appeared that way to me. Help me to understand where i went wrong.
Either way, its better safe than sorry and better to just do a quick code 3 transport and have it NOT be one than not treat it like that and miss it.....
but just an education moment for me! THanks guys.
