First of all... All excellent posts and suggestions. This was an intentional hard case I had....
Since this location is on outskirts of town, you have a return trip to the hospital of 15 minutes .. dependent on time and traffic.
You quickly review the assessment and hx. again.. attempting to narrow this complex situation. You again quickly ask the husband how much vomiting, diarrhea.. etc. He informs you he didn't think that she had than many episodes, but she told him that her head was hurting her and she was going to take some more of her headache medicine. Being the astute Paramedic you are, reviewing the unusual fasciculations, cardiac ectopi, and sudden B/P you as well initially assume neuro or dehydration, but so severe? You ask how if she was on any other headache medication and he informs you that she was not, she used to be on Imitrex but was not on effective. So they placed her on this one which appeared to work "a bit better".
You look at the medicine and note that the headache medication is Doxepin ? Not being familiar with this you pull out your handy-dandy pocket field guide & look it up.
BINGO !... It now makes sense!.. Doxepin is a tetracycline antidepressant that is widely used for migraines.... tetracycline/anticholinergic poisoning!. ..Neuro irritability (fasciculations) initially salivation now dry.. slightly erythematous flushed skin, arrhythmia's tachy to wide complexes.. she apparently self medicated herself additionally and with the additional antihistamine from NyQuil and caffeine and dehydration she has made herself a life threatening cocktail. As well she is very petite and low body mass and excellant metabolism does aid in absorption of medication .
You immediately establish fluid resuscitation and initiate a Dopamine drip at 6-8 mcg/kg/min as well drop a large oral gastric tube with irrigation of saline. You note some small pill fragments on return ...
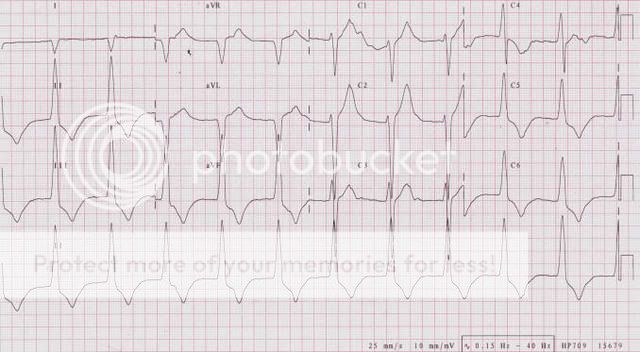
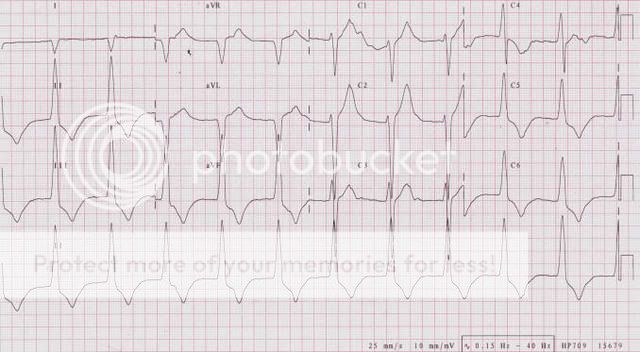
ECG remains as noted but you do see some attempts of conversion with occasional sinus beats. Her pressure with fluids and Dopamine has reached 82/58 and her respiratory rate has increased a little.
You arrive in the ED and the ER Doc agrees with your speculation. A serum level is drawn as well as tox screen and cardiac profile and the usual other routine lab's. The patient is placed on ventilator and radiography films are taken as well as an emergency brain to pelvic CT scan.
You had to respond to another call but able to return about 2 hrs later.
The patient is being packaged and prepared for transfer to ICU.
The Doc personally comes to talk to you and pats you on the back and congratulate you on a job well done!. Her lab's is a train wreck with BUN and anion gap horrible showing severe dehydration. As well, her tox level initially was high but not severely dangerous.. but as the physician describes along with the other factors potentiated the tetracycline. CT is negative as well as cardiac markers .. except her CPK probably due to your cardioversion.
She was placed in the unit for consideration for emergency dialysis but due to severe dehydration was postponed. She regained consciousness about 8 hours later and ventilator was discontinued the next morning. She was rehydrated and discharged three days later, of course a change in medication. ..lol
Lesson learned... when one hears hoofsteps..don't always assume it is horses.. it might be zebras!
Multiple indications for medications can be confusing, i.e. NTG for esophageal spasms, Haldol for headaches.. etc.. Not only can trauma/medical patients can have multiple problems, medical patients can as well. Sometimes it appears they attempt to "test" our capabilities all the time.
Again, good going guys! Great responses.. !
R/r 911