Typing... too... many... words... need coffee. COFFEE.
Thanks, that makes sense.
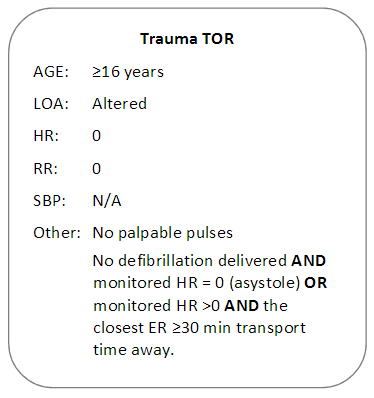
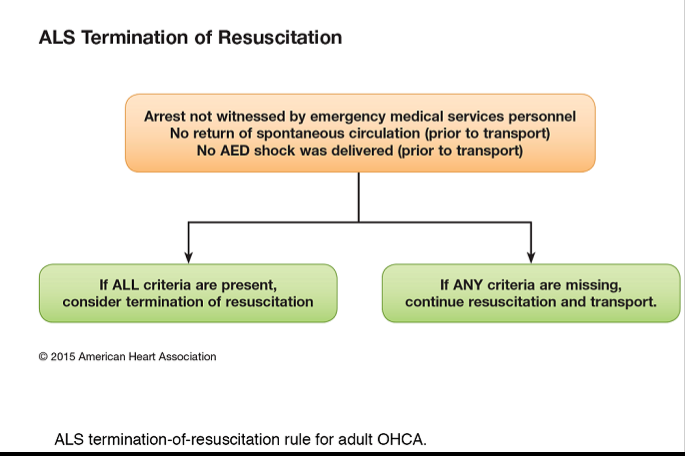
I don't really understand your question. We transport every medical arrest that is non-cardiac in origin or do not meet our medical/trauma termination of resuscitation guidelines. As for point c), shouldn't we always be able to transport with CPR enroute if they meet transport parameters? There usually would be Fire tagging along for 2 person CPR while your partner is driving or just do one-person CPR until you meet up with another crew if transport is long enough.
We'll work it and call it with no response. Aside from a set of "they can fix it, we can't" discussed above, there isn't any need for transporting, especially without a transport CPR device (Lucas, etc...). If it's just two of you, seriously, two man CPR until you get help. One provider CPR in the back of a moving, bouncing truck is hideously bad, highly ineffective and is way more likely to get the one in the back hurt. Your scope of practice, protocols and "Mother, may I?" can differ than ours.
Toxicological, unlikely. Not unless you have a clear agent and a clear antidote which is not available prehospitally AND transporting would not place the crew at risk of a secondary exposure, AND if the hospital actually has it readily available. If they die from ingesting cyanide crystals, they're dead unless you get an antidote in them _now_ and not at the hospital in 10-45 minutes. Black mamba bites, yeah.. if they already died, they're dead. Methylethylyukkyshit, if they're dead before they're deconned... see where this is going?
Anaphylaxis? Unless something went very wrong, we best be having epi on board (first line), although given the arrest methodology I might be adding a few more meds into the cardiac arrest matrix. Past the IO/IV adrenaline, for the airway edema we have nebulized epinephrine and salbutamol. For anaphylaxis we have a liter of fluid, more epi, yet more epi, diphenhydramine, hydrocortisone, and phenylephrine.
Foreign body you can't clear? Can your ER do an emergency tracheostomy on arrival within 2 minutes? Most can't...
Not to mention the newer studies showing you should wait a few minutes after ROSC rather than immediately running to the hospital while the Pt hopefully stabilizes and could re-arrest during extrication and not be noticed.
Clinical hypothermia (which isn't terribly common here, even in winter), select trauma, STEACS/ MI codes that can go straight to the cath lab, pregnant, or working organ donors that police aren't going to hold the body on. Pediatrics is a common "transport no matter what" cardiac arrest. It is, however, worthless clinically while helping to hurt the family emotionally (false hope), getting more family and EMS hurt (MVA, ongoing compressions enroute) while also functioning as an in-writing policy for age discrimination against older patients.