Ah, you were catching on that I was posting name that ECG here.
Rate? 167-187. I trust the monitors HR which is 176.
Regularity? Regularly regular
P-waves? Yes. I think it's best seen in lead I. I can see it in V4-V6. Would be questionable in V2-V3, but with the other leads, I would say those notches at the end of the T-waves aren't artifacts, but p-waves superimposing on the T-wave making a notch.
Arrows pointing at notch.
PR interval? Hm, not sure if it's consider calculable. I decided to use lead II. The second half of what I would call the T-wave is very tall (like when there is LAE or RAE, since both atrias are depolarizing at the same time and one has more surface than the other, it makes a tall p-wave; I know people say p-pulmonale, the tall p-wave >2.5 mm is RAE, but I believe I read that it's non specific for which one it is per Chou's book in the first few chapters I read (haven't read the whole thing). I am applying the same idea, but with a T-wave instead). I would say in II, it looks like 0.12s. Looking at the other leads, it's like 0.08s, but like what Garcia's book said, it's the longest that counts.
Arrow pointing at notch, all of the sudden it gets bigger cause of combined electrical activity.
QRS duration? 0.04s
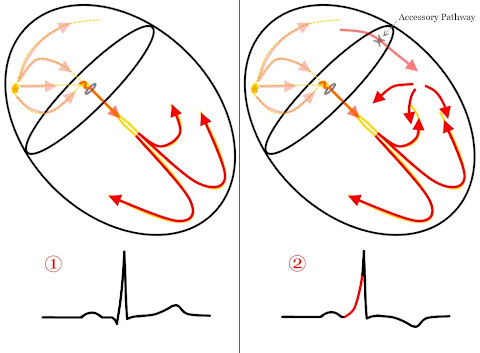
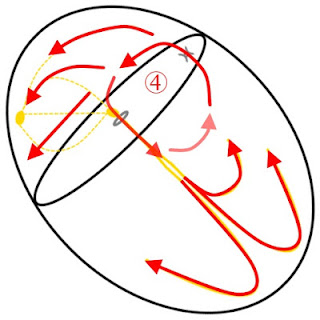
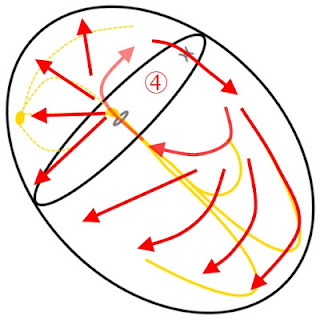
Rhythm DDx? Well, it's obviously an SVT, and I just happened to read from
ems12lead the different types of rhythms and SVT can be: sinus tachycardia, atrial fibrillation, atrial flutter, atrioventricular nodal re-entry tachycarda, accessory pathway mediated tachycardia, atrial tachycardia, multifocal atrial tachycardia, and junction tachycardia. Sinus tachycardia is a possibility. It's regularly regular so not atrial fibrillation. I would expect to see flutter waves between the T-wave in the inferior leads since there is some gaps in there (and atrial flutter is usually best seen in the inferior leads and pointy T-wave in V1 I recall). AVNRT is still new to me so I am not sure. Also with accessory mediated, I think it's talking about WPW, and I don't see any delta wave (I try not to look too hard at the 12-lead, lol) and if I am correct about the PRi then no. Atrial tachycardia is possible if I am incorrect about the PRi and whether the P-waves are positive/negative. Where I am seeing P-waves, it looks positive in I, II, III, and aVF (makes the T-wave peaked). It's regularly regular so not multifocal atrial tachycardia either. It has a P-wave so it's not junctional tachycardia either. I think it's sinus tachycardia even though it's questionable with that rate.

This is in regard to me not seeing any flutter waves in the inferior lead.
Axis? QRS: I is positive, aVF is positive. This is in the normal axis. If you use the I, II, III trick, I is positive (it's going to the patient's left), II and III are positive (it's going down) so it's going down and to the left, which is normal. aVL is most isoelectric/equiphasic so I would say around +60 degrees. Z: V3-V4 are equiphasic so +20 - +40. Normal R-wave progression.
QTi/QTc? Once again, I am not sure if considered calculable. Since the atria is depolarizing almost simultaneously as the the ventricle is repolarizing, I'd say to assume that calculating it even with the P-wave inside of it is OK. QT is about 280 ms. QTc is about 479 ms (280/((60/176)^(1/2), I trusted the monitors HR).
ST/T-wave changes? I don't see anything in the inferior leads (that have a gap before the T-wave) It's difficult to tell since I really don't a good TP segment to use and going off of the PRi instead. In tachycardias, sometimes it looks like there is ST depression because the atrial is repolarizing after the ventricle depolarize I think. I don't think the P-wave in V1 could be negative enough to make it look like retrograde T-waves so maybe retrograde T-wave in V1, but that's all.
Overall DDx? No (bad word)ing clue.

Dehydration caused by something like an infection is all I'm thinking. If that's the case, fluid resuscitation would be better than administering adenosine since this tachycardia is compensating/terminating the rate without more fluids would be harmful. I cannot think of anything else that I would associate with this 12-lead.