Christopher
Forum Deputy Chief
- 1,344
- 74
- 48
52 year old male, called 911 because he has felt "sick and weak" and doesn't seem to be getting any better.
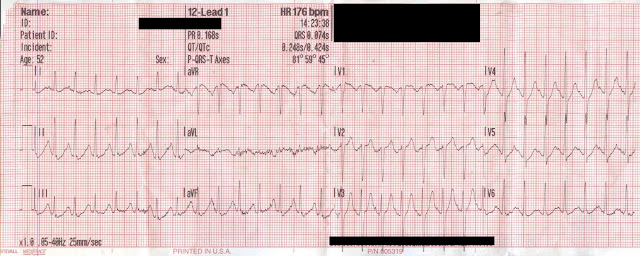
(click image for larger version)
You ain't getting anything else, but I'd like a rhythm interpretation
Rate?
Regularity?
P-waves?
PR interval?
QRS duration?
Rhythm DDx?
Axis?
QTi/QTc?
ST/T-wave changes?
Overall DDx?
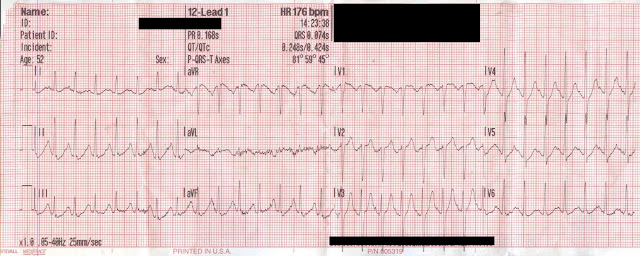
(click image for larger version)
You ain't getting anything else, but I'd like a rhythm interpretation
Rate?
Regularity?
P-waves?
PR interval?
QRS duration?
Rhythm DDx?
Axis?
QTi/QTc?
ST/T-wave changes?
Overall DDx?
