- 5,055
- 1,476
- 113
Yes, the old rules of injury patterns and vehicles don't apply... because people are wearing seatbelts more often and interiors of vehicles are much better designed to reduce injury by absorbing energy when impacted. This has the effect of reducing the forces that are applied to the body during a MVC. The same rules of knowing injury patterns still does apply though. If you do not know where and how energy is transferred between objects, the best you can do is guess that the body sustained a significant impact...Just about any road traffic collision these days. The idea of MOI as being predictive arose in the 60s and 70s, when the white paper on trauma was put together. I guess it may have been considered predictive at that stage because you would have repeatable patterns of injuries seen in motor vehicle collisions as heads hit windscreens, chests hit steering wheels, knees hit dashboards and so on.
With advances in design and engineering in vehicles now those same rules do not apply. They don't even apply to pedestrian impacts as vehicle manufacturers work on minimizing injuries to pedestrians as well.
MOI is not prognostic in any way, the only thing it is good for is to alert you to the potential for there to be injuries.
I suspect Vene's point is that we see and understand so little of the process of managing trauma in the ambulance. The actual management of trauma, as opposed to just delivering trauma to the hospital, is enormously complex and difficult.
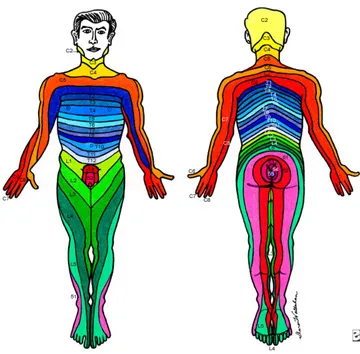
Mechanism is very, very poor at predicting presence of actual injury, but it is very good at "showing" where injury is likely to occur. If you get struck in the head by a rock, I'm not going to look at your feet to see if your toes were broken or dislocated by the impact your head sustained. In that regard, I'm probably not going to look any further "south" than C7-T1.
You really don't, and can't, get a good understanding of this kind of stuff in a short merit-badge trauma course.
The human body is a remarkably tough and fragile thing. Apply stress in just the wrong place in the wrong direction, and things can break spectacularly easily... yet apply the same amount of force to the body in a different direction and you'll see no evidence of injury because there is none to be found.