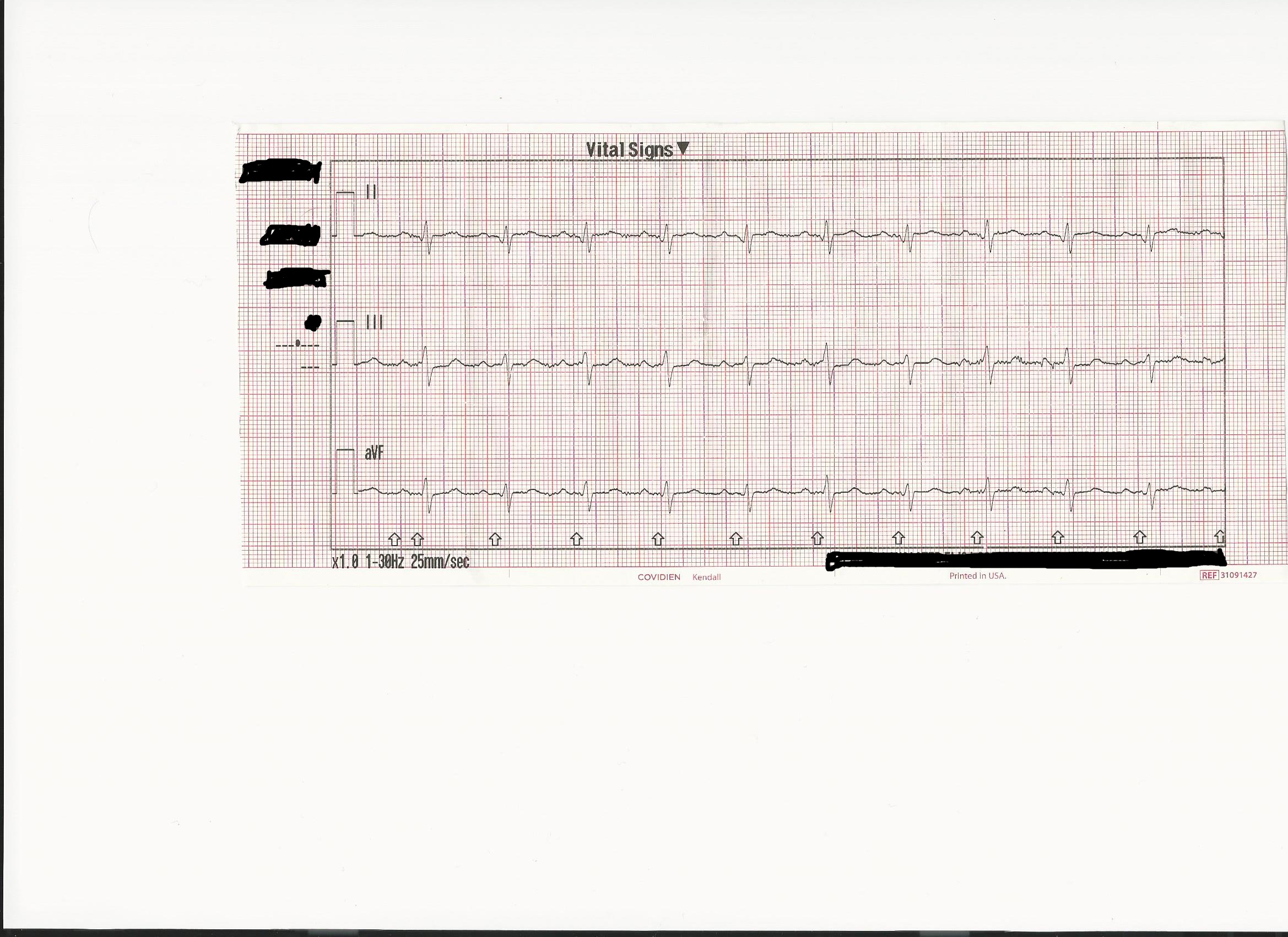
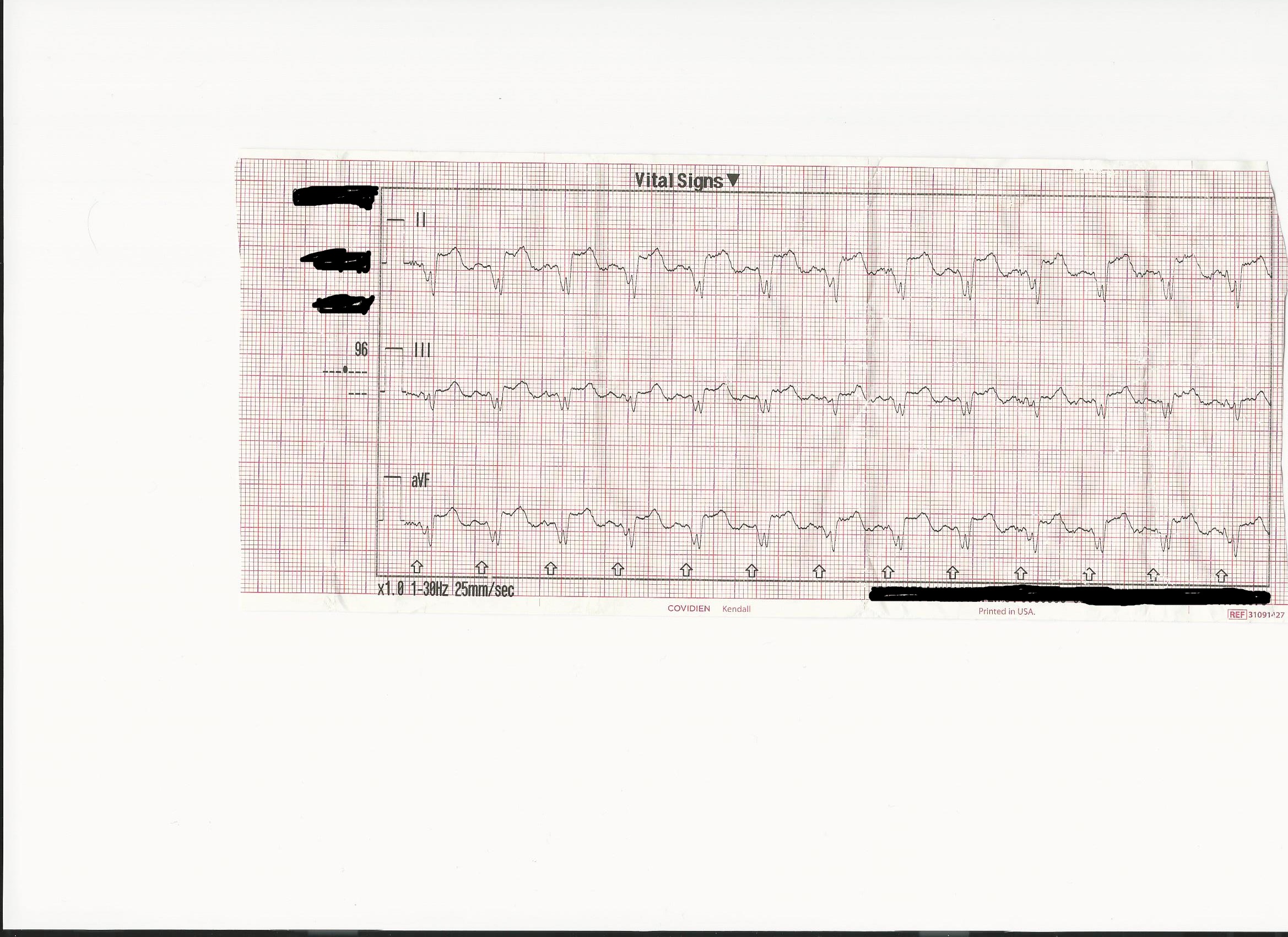
Are they so massive? If we ignore the rhythm strips it's not so dramatic.
I'm with Brandon on this one.
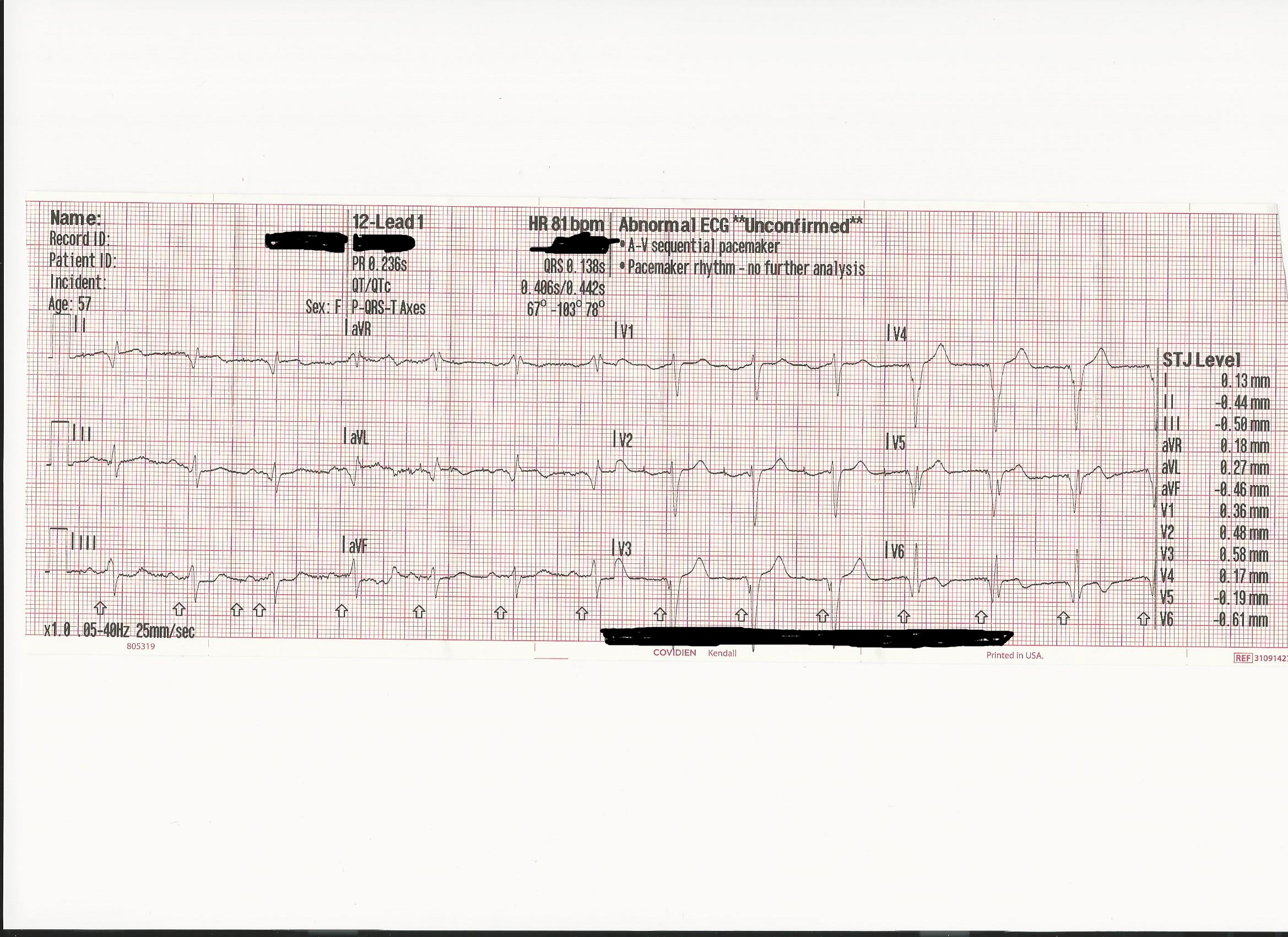
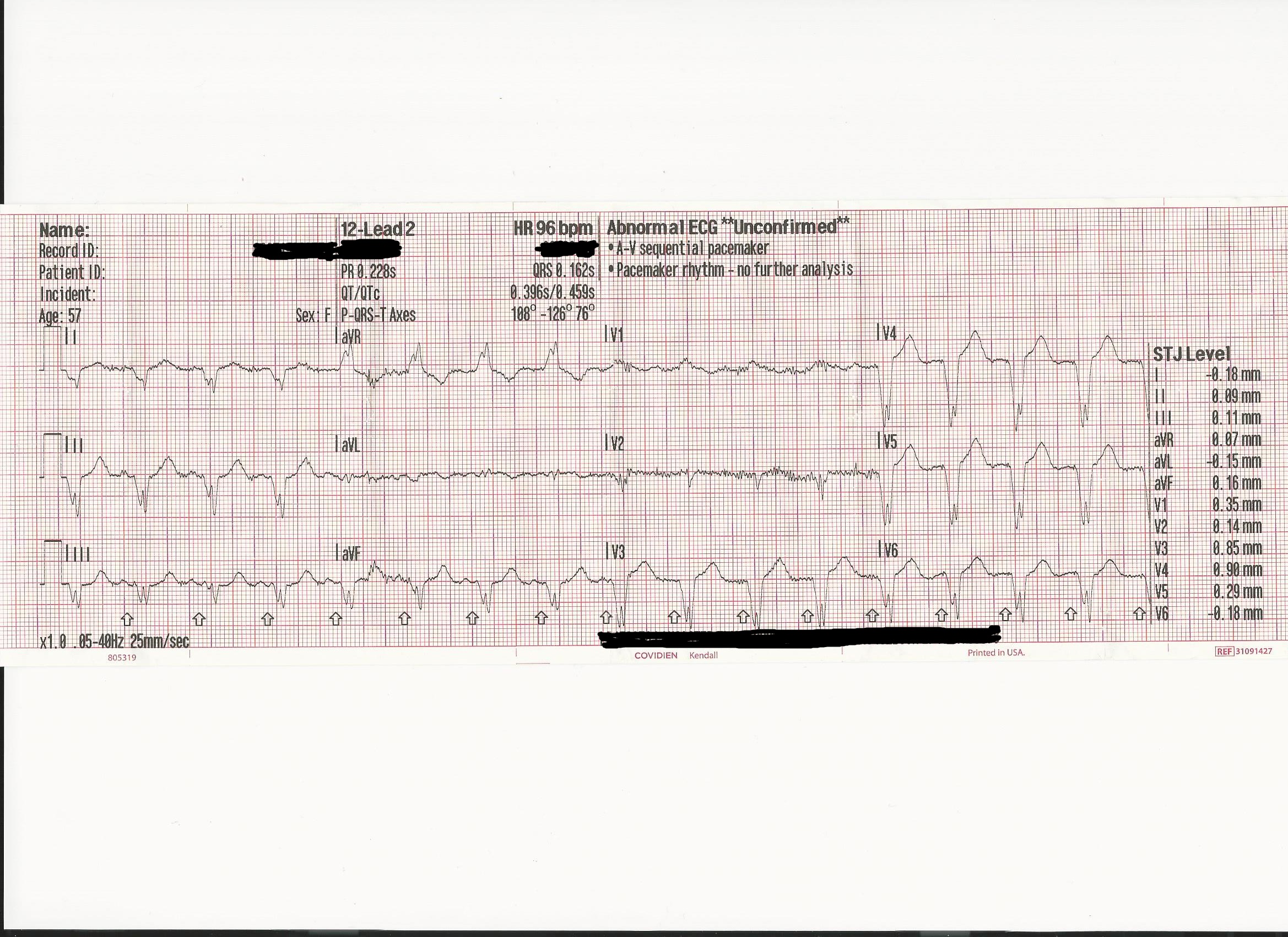
These ECG's read identically, just like the monitor says. Remember that reading an ECG is not about pattern recognition. Just because the patterns of the tracings don't look like the same thing doesn't mean that the ECG's don't read the same.
First off, rhythm strips are not for morphology interpretation. Monitors have a different filtering and amplification algorithm for the rhythm display and the diagnostic 12 Lead. The rhythm strip is the "Non Diagnostic Mode", that's why it takes a moment to process a 12 lead. Can you sometimes see nice big tombstones on lead II? Sure, but even someone with the worst, blurriest vision can point out a huge mountain on the horizon, they can't tell you if it's snow capped though. That's an apt analogy, the rhythm strip is literally a lower resolution than the 12 lead.
If we compare the two 12 leads they are identical, if of different overall voltages, including a non-diagnostic tracing in v1 and v2 as well as aVL on the second. When you look at them side by side the morphology is the same, the center of each complex has just been pulled up or down respectively. The increase in amplitude is due to the 12 Lead warming up.
Ok, that was a joke, sorry. When I learned about this from my preceptor he told me a story about a 12 Lead class he was once in where a medic asked the instructor;
"Why does it sometimes take five or so minutes for my ECG to 'warm up' and the artifact to go away and the tracing be clear?"
Everyone looked at her like she was crazy, but it's true. Not that the 12 Lead warms up, but the gel on the electrodes is water soluble. We put the electrodes on the "skin" but really the outermost or "horny" layer of the skin is extremely hydrophobic, while just under it the dermis is extremely hydrophilic. The electrode gel at first only comes into contact with the "horny" layer made up of sebum, oils, and dead dermal cells among other non-living stuff. This isn't enough impedance to completely keep the ECG from seeing the electrical signals of the heart but it is enough to dampen them. That's why you have lower voltage in your first 12 Lead. After three to five minutes the electrode gel has dissolved much of the water soluble materials and seeped down to come into more complete contact with the dermis and thereby the patients total body water compartment, where all the electrical activity happens. Now you have a much clearer picture but you are seeing a lot more artifact, which is to be expected. Additionally I would guess the second 12 Lead was done with more general movement of the patient? Maybe in the back while driving? We lost diagnostic tracings completely on V1, V2, and aVL, so maybe the electrodes aren't adhering well? Are the electrode on the extremities? You always want the electrodes on the shoulders and chest.
For further proof of this you have to look only as far as the stress test lab. Those cats get awesome 12 leads on people on freaking stairmasters and I have my medic students tell me the artifact from the road is too much to overcome.... Something is up. The trick turned out to be super fine grit sandpaper made by 3M. I asked a cardio tech. friend about it and he said they sand the skin down so it's slightly red and raw before putting the electrode on. Bam, near perfect ECG's (chest and abdomen, no extremities! ECG's literally can't see extremities, it's a mathmaticall sphere and you're just putting the "camera" further away.) Always shave off all hair and the I use a damp 4x4 to rub the spot raw. I haven't been able to convince anyone to buy my sandpaper yet, but someday.
With the 12 leads above they read identically, if we were evaluating them for ischemia / infarct (we have a paced rhythm so we're going to use the scarbosa(sp?) criteria) we get a negative assessment for signs of ACS in both ECG's, and in the leads we can compare (v3 for example) that have diagnostic tracings both times the read according to the scarbosa(sp?) criteria is pretty much without change.
Anyway, like Brandon brought up in order to discuss this someone is going to have to point out how the 12 Leads are different other than overall amplitude.
What interested me more in your post was that you seem to know, or have been taught that it would be normal for CPAP to induce ECG changes. I haven't ever read that, could you provide a source that talks about that happening? I'm not convinced that it couldn't but I can't really talk about it without knowing more about it, I couldn't turn up much on google either.
Electrophysiology is one of my favorite topics so I'll say what I THINK might be how it should work, but I'm kind of hoping I'm wrong here cause this sounds interesting.
CPAP should not, in an otherwise healthy heart induce any ECG changes that are not secondary to the possible increased oxygenation of the heart. It is well documented however in research on Obesity Hypoventilation Syndrome / Sleep Apnea that CPAP is capable of eliminating transient ST changes associated with hypoventilation induced hypoxia. So where I come out of it is; although it is documented that CPAP could enact ECG changes in relation to restoring oxygenation to the heart thereby directly relieving ischemia and it's corresponding ECG changes, we wouldn't expect any change in an ECG not related to that relieved ischemia. I just can't think of an electrophysiologic mechanism by which we would expect CPAP to cause primary ECG changes.