- 4,549
- 3,291
- 113
Yet it certainly happens. While EMS probably wasn't at fault when the big burn ends up 15 liters overrescuscitated during the first 24 hours, the 4 liters they give in the field probably didn't help. Some sense for the initial goal volumes (which will be titrated going forward, but mostly via criteria like urine that we don't follow in the field) is helpful to get in the middle of the not enough-too much range.
You'll always be able to find extreme examples of outliers, but I don't think they make a good argument against a simplified approach to IVF administration in these patients. If anything I think they support the need for it. I would advocate something along the lines of 2 liters as fast as reasonably possible and then 1 liter per hour. With transports well over an hour or in certain patients that rate could certainly be adjusted, but I think it makes a nice simple starting point that everyone can understand and be on the same page about and it minimizes the chance of massive over or under resuscitation.
The last HEMS program that I worked for had a contract with a regional burn center that received patients from several surrounding states. We picked up many burn patients from both scenes and hospitals large and small to take them to the burn center. IME, little causes more confusion and miscommunication than how much IVF the patient has gotten and should get. From EMS to the first ED to the burn surgeon's PA to us and then back to the burn surgeon again (who we took med control from for these transports), no one was ever on the same page, and it was very common for these patients to get way too much or way too little IVF. There should be a simpler way.
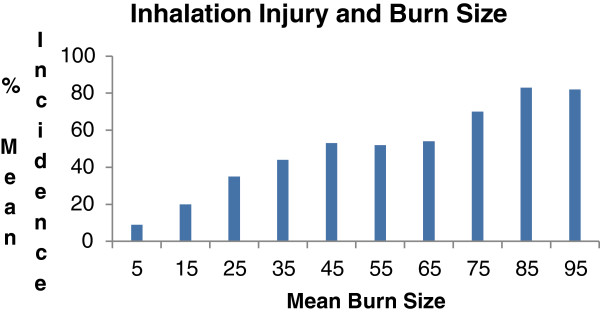
True thermal injury to the lower airways are uncommon, but inhalation injury from other causes (such as direct toxicity from smoke inhalation) is common, and massive fluid resuscitation alone is an indication for intubation (as is, arguably, heavy sedation). It doesn't have to be done in the field as I agree that you often have something of a grace period before the airway really poops out on you, but it should be managed as soon as it safely can be.
This I think just depends on your basic attitude towards prehospital RSI. Folks who support aggressive RSI in the field will find plenty of ways to justify intubating many of these folks at the scene. Those of us who favor a more measured and conservative approach to prehospital RSI however, feel as though just because a large number of these patients end up intubated eventually does not argue for doing it in the field. When these patients get intibated it is almost always due to systemic edema that develops over the first days and/or because of high narcotic requirements and repeated debridements. Upper or lower airway burns causing early airway edema is actually quite rare, even when the classic signs that we are taught to look for exist.
Last edited: