Navigation
Install the app
How to install the app on iOS
Follow along with the video below to see how to install our site as a web app on your home screen.
Note: This feature may not be available in some browsers.
More options
Style variation
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Whats the significance of controlled hyperventilation?
- Thread starter patzyboi
- Start date
Ewok Jerky
PA-C
- 1,401
- 738
- 113
Never heard of controlled hyperventilation.
As for controlled hypertension, I assume you are referring to htn that is controlled with medication. In that sense, you should know what medication they are on, possible side effects such as cough, low K+ etc. And sequela such as left ventricular hypertrophy, CAD, renal and heart failure etc.
Should you u be concerned about it at the basic level? Depends on of you want to stay a basic forever
As for controlled hypertension, I assume you are referring to htn that is controlled with medication. In that sense, you should know what medication they are on, possible side effects such as cough, low K+ etc. And sequela such as left ventricular hypertrophy, CAD, renal and heart failure etc.
Should you u be concerned about it at the basic level? Depends on of you want to stay a basic forever
Ewok Jerky
PA-C
- 1,401
- 738
- 113
In that sense he be referring to permissive HTN in the setting of stroke. Generally accepted to allow SBP of 180 to maintain perfusion during a brain bleed.
Maybe he is talking about purposely hyperventilating to decrease intracranial pressure? It is no longer recommended.
In that sense he be referring to permissive HTN in the setting of stroke. Generally accepted to allow SBP of 180 to maintain perfusion during a brain bleed.
Probably want the pressure a little lower than that for a bleed. However, 180 is very reasonable for an ischemic stroke.
Ewok Jerky
PA-C
- 1,401
- 738
- 113
Oops my bad, good thing I went into ortho.Probably want the pressure a little lower than that for a bleed. However, 180 is very reasonable for an ischemic stroke.
ThadeusJ
Forum Lieutenant
- 240
- 69
- 28
As APRZ stated above, they used to hyperventilate patients to lower the PCO2 which had been found to decrease intracranial pressure. Later studies indicated that it didn't do a whole heck of a lot, was a temporary fix and may have even had deleterious effects. So this treatment has been questioned for a couple of decades now.
However, please do not confuse hyperventilation (breathing at a rate and volume to lower the PCO2 level to result in a respiratory alkalosis) with tachypnea (breathing above a normal respiratory rate). Patients suffering from a metabolic acidosis (renal failure, ketoacidosis secondary to diabetes) will increase their respiratory rate to compensate for the drop in pH. This tachypnea lowers the PCO2 and therefore increases the pH back into a normal range. There are many people out there who feel the need to sedate the patient to make them appear normal but unwittingly cause them to drop their pH to dangerous levels. Don't be one of them.
However, please do not confuse hyperventilation (breathing at a rate and volume to lower the PCO2 level to result in a respiratory alkalosis) with tachypnea (breathing above a normal respiratory rate). Patients suffering from a metabolic acidosis (renal failure, ketoacidosis secondary to diabetes) will increase their respiratory rate to compensate for the drop in pH. This tachypnea lowers the PCO2 and therefore increases the pH back into a normal range. There are many people out there who feel the need to sedate the patient to make them appear normal but unwittingly cause them to drop their pH to dangerous levels. Don't be one of them.
teedubbyaw
Forum Deputy Chief
- 1,036
- 461
- 83
Hyperventilation causes vasoconstriction. This was thought to better perfuse the brain in a head injured pt, however, vasoconstriction does quite the opposite in that case. It is still within many protocols to slightly hyperventilate.
Anthony7994
Forum Crew Member
- 32
- 0
- 6
Hyperventilation causes vasoconstriction. This was thought to better perfuse the brain in a head injured pt, however, vasoconstriction does quite the opposite in that case. It is still within many protocols to slightly hyperventilate.
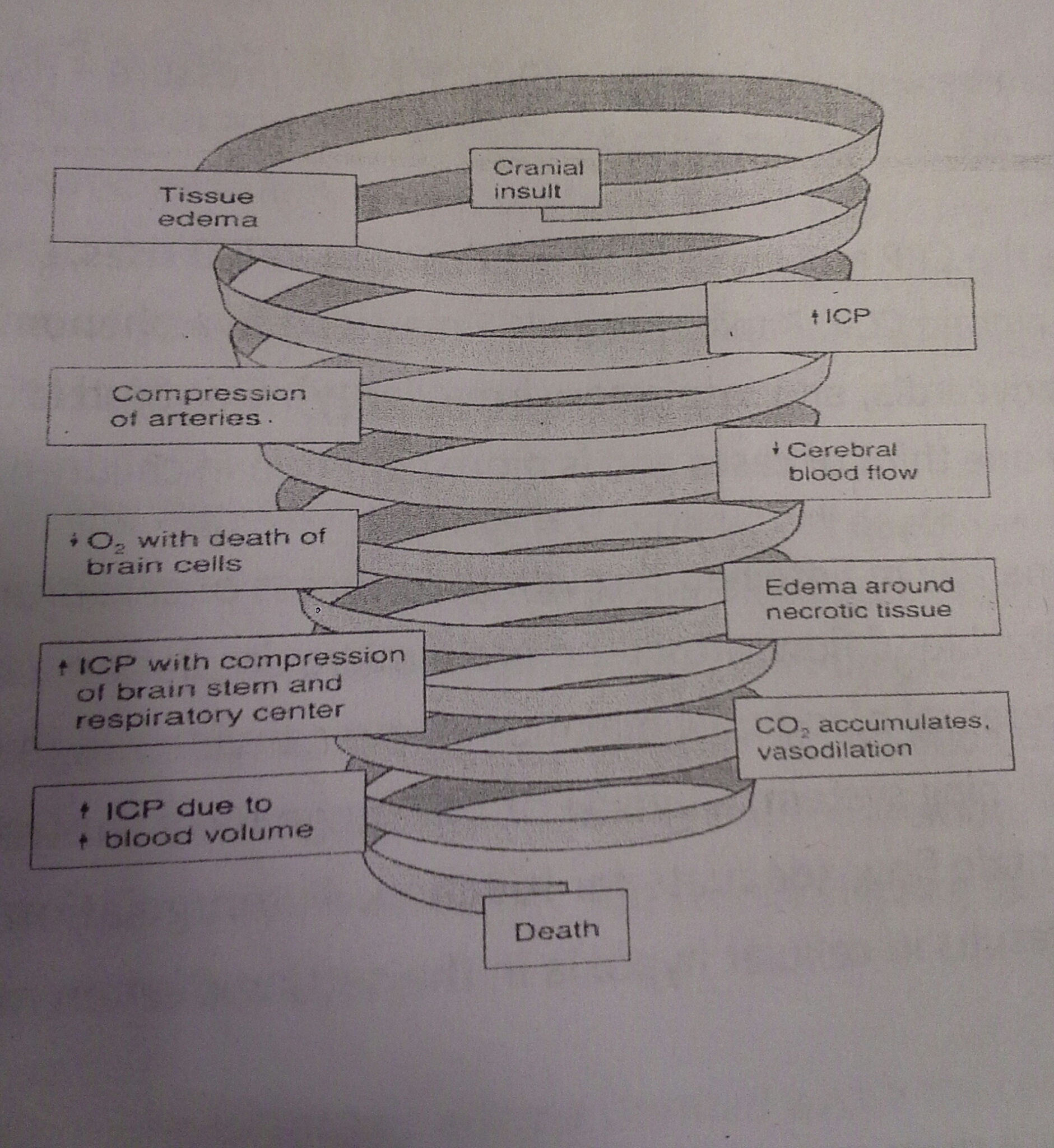
I thought that the hyperventilation was to decrease the ICP? From what I had gathered an increase in CO2 causes vasodilation which increases ICP. The "permissive hyperventilation" (an EtCO2 of 30-35) helps reduce that. But, the CO2 would come from respiratory acidosis in the late phase of a TBI with herniation, so it seems to really be a last-ditch-effort so to speak. Just my two cents.
Anthony7994
Forum Crew Member
- 32
- 0
- 6
I was in a class a couple of years ago that a neurologist taught us about treatment of TBI in the field (military setting). We got a huge packet on it that I still keep as a reference, and is a picture in it that helps with what I said.
- 2,735
- 1,272
- 113
I thought that the hyperventilation was to decrease the ICP? From what I had gathered an increase in CO2 causes vasodilation which increases ICP. The "permissive hyperventilation" (an EtCO2 of 30-35) helps reduce that. But, the CO2 would come from respiratory acidosis in the late phase of a TBI with herniation, so it seems to really be a last-ditch-effort so to speak. Just my two cents.
I think you and teedubbyaw are saying the same thing here. Increased levels of CO2 do cause vasodilation, so hyperventilation and forcibly decreasing the EtCO2 and PaCO2 were thereby theorized to result in vasoconstriction.
The reality is that like everything else in medicine it isn't that simple. Even moderate hyperventilation (30-35 mm Hg EtCO2) can result in decreased cerebral blood flow due to the ensuing vasoconstriction and thusly potentially causing cerebral hypoxia. In the great scheme of TBI care, increasing ICP is bad, but increasing cerebral hypoxia is really bad. There are some arguments that injured brain tissue has decreased metabolic and O2 demands in its post injury state, but that is why any hyperventilation is only recommended in cases where increasing ICP is 100% confirmed and the hyperventilation/cerebral perfusion balance can be maintained in a critical care setting.
Even brief episodes of hypoxia (iatrogenic errors clearly included here) have a devastating effect on morbidity and mortality of severe TBI patients. This is why the possible benefits of slightly decreasing ICP is not judged to be worth the risk of cerebral hypoxia with EMS initiated hyperventilation. Our current guidelines instruct us to titrate ventilation rates to EtCO2 values of 40-45 mm Hg in TBI patients.
SandpitMedic
Crowd pleaser
- 2,309
- 1,260
- 113
I think you and teedubbyaw are saying the same thing here. Increased levels of CO2 do cause vasodilation, so hyperventilation and forcibly decreasing the EtCO2 and PaCO2 were thereby theorized to result in vasoconstriction.
The reality is that like everything else in medicine it isn't that simple. Even moderate hyperventilation (30-35 mm Hg EtCO2) can result in decreased cerebral blood flow due to the ensuing vasoconstriction and thusly potentially causing cerebral hypoxia. In the great scheme of TBI care, increasing ICP is bad, but increasing cerebral hypoxia is really bad. There are some arguments that injured brain tissue has decreased metabolic and O2 demands in its post injury state, but that is why any hyperventilation is only recommended in cases where increasing ICP is 100% confirmed and the hyperventilation/cerebral perfusion balance can be maintained in a critical care setting.
Even brief episodes of hypoxia (iatrogenic errors clearly included here) have a devastating effect on morbidity and mortality of severe TBI patients. This is why the possible benefits of slightly decreasing ICP is not judged to be worth the risk of cerebral hypoxia with EMS initiated hyperventilation. Our current guidelines instruct us to titrate ventilation rates to EtCO2 values of 40-45 mm Hg in TBI patients.
Great input. Cerebral hypoxia is the worst,as you said.
It will flat out kill the patient... and nothing else you do will matter.
Regarding the picture posted... It is pretty much the illustration we should all be thinking... ICP increases, cerebral blood flow (oxygenation) decreases, and it is a vicious spiral out of control. The evidenced based medicine on the effects of titrating the EtCO2 (ultimately PaCO2) to permissive respiratory alkalosis has not yet been disproved on the mainstream level. I remember though, during my initial paramedic clinicals in the TICU, I asked a Trauma Doc the same question... He pretty much told me exactly what Chaz said.. It doesn't help, and is likely doing more harm than good. But that is what we do in EMS... figure out the best practice.
Flying
Mostly Ignorant
- 571
- 370
- 63
That is a neat little picture, is there an original source you can point to?I was in a class a couple of years ago that a neurologist taught us about treatment of TBI in the field (military setting). We got a huge packet on it that I still keep as a reference, and is a picture in it that helps with what I said. View attachment 2229
Last edited:
Anthony7994
Forum Crew Member
- 32
- 0
- 6
I really wish I could. I've searched for it frequently and can't find it. The presentation handout was made by the neurologist herself, so I've still held onto that packet like gold.That is a neat little picture, is there an original source you can point to?
