chico.medic
Forum Crew Member
- 61
- 0
- 0
I was wondering if anyone had diltiazem(Cardizem) in their scope of practice. (I'm talking about EMS systems- Pre-Hospital.)
I realize that being a calcium channel blocker there are several considerations when administering the drug for tachycardias (Administration of diltiazem with digoxin can increase digoxin blood levels. Therefore, blood levels of digoxin are usually monitored to avoid toxicity. Similarly, concurrent administration of diltiazem with an anti-seizure medication carbamazepine (Tegretol) can increase blood levels of the seizure medication, and occasionally lead to toxicity. Concurrent administration of cimetidine (Tagamet) interferes with the liver breakdown of diltiazem, and significantly increases diltiazem blood levels. Therefore, cautious dosing is necessary when both medications are administered.) It can also cause a worsening of heart failure.
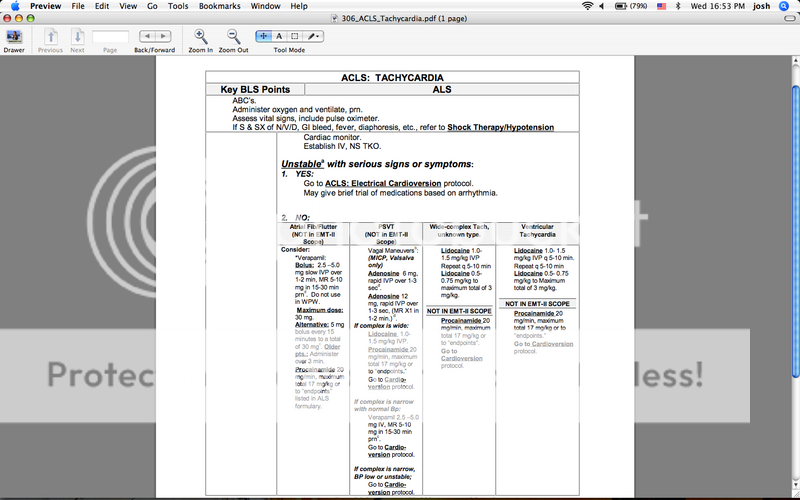
The reason I bring it up is I had a patient today in a Narrow Complex Tachycardia that resembled PSVT @ a rate of 180 BPM. His BP was 104/60, R-22 mildly labored, SAo2%-96 on room air. He had had a sudden onset of sub-sternal chest pressure radiating down his left arm about 20 minuets PTA. 10/10 on a pain scale. He was Alert & Oriented, GCS was 15. His skin was slightly pale, warm and moist. I administered Adenosine and that was enough to slow the rate to see that it was a Rapid Atrial Tachycardia. Seeing as Adenosine is not very effective on Atrial Tachycardias, the only other drugs we have in our protocols are Procainamide (Which is impractical to set up with short transport times,) and Verapimil.
Verapimil has fallen out of favor, and I see Physicians using Cardizem more frequently, at least in this area. So if it is proven to be so effective in the hospital setting, why then is it not favorable for use in the field?
I realize that being a calcium channel blocker there are several considerations when administering the drug for tachycardias (Administration of diltiazem with digoxin can increase digoxin blood levels. Therefore, blood levels of digoxin are usually monitored to avoid toxicity. Similarly, concurrent administration of diltiazem with an anti-seizure medication carbamazepine (Tegretol) can increase blood levels of the seizure medication, and occasionally lead to toxicity. Concurrent administration of cimetidine (Tagamet) interferes with the liver breakdown of diltiazem, and significantly increases diltiazem blood levels. Therefore, cautious dosing is necessary when both medications are administered.) It can also cause a worsening of heart failure.
The reason I bring it up is I had a patient today in a Narrow Complex Tachycardia that resembled PSVT @ a rate of 180 BPM. His BP was 104/60, R-22 mildly labored, SAo2%-96 on room air. He had had a sudden onset of sub-sternal chest pressure radiating down his left arm about 20 minuets PTA. 10/10 on a pain scale. He was Alert & Oriented, GCS was 15. His skin was slightly pale, warm and moist. I administered Adenosine and that was enough to slow the rate to see that it was a Rapid Atrial Tachycardia. Seeing as Adenosine is not very effective on Atrial Tachycardias, the only other drugs we have in our protocols are Procainamide (Which is impractical to set up with short transport times,) and Verapimil.
Verapimil has fallen out of favor, and I see Physicians using Cardizem more frequently, at least in this area. So if it is proven to be so effective in the hospital setting, why then is it not favorable for use in the field?
Last edited by a moderator: