jedirye
Forum Lieutenant
- 114
- 0
- 0
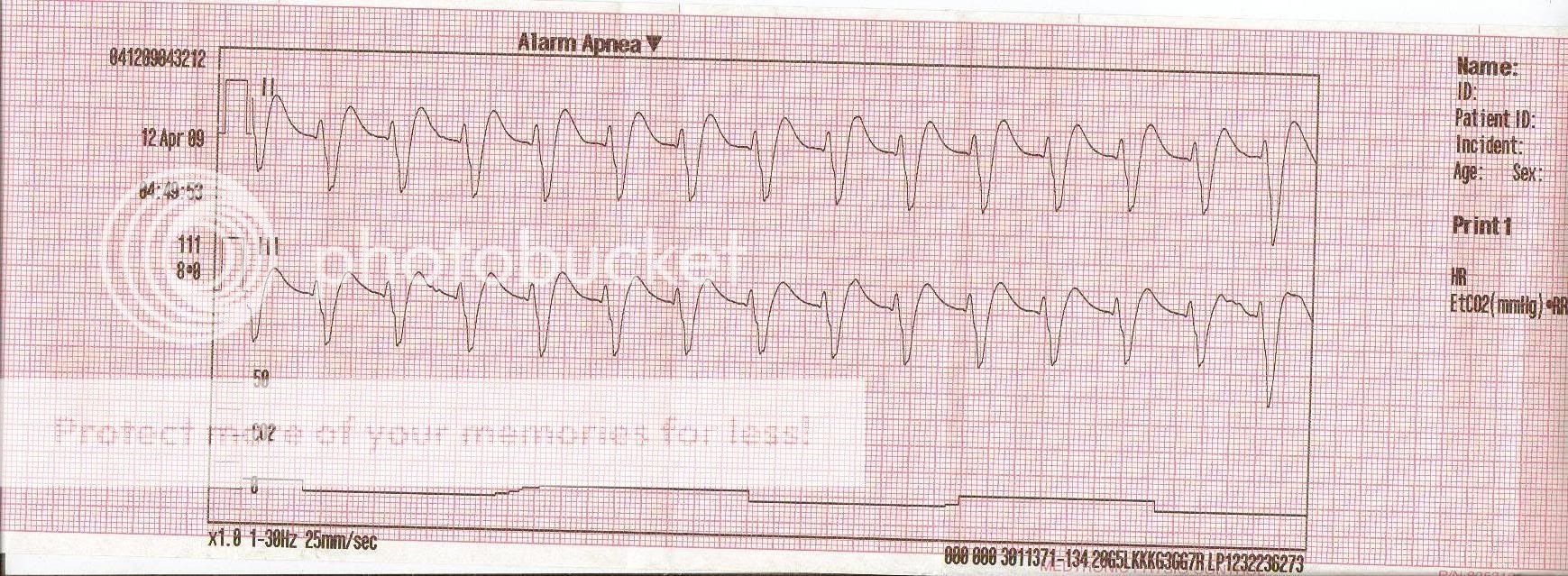
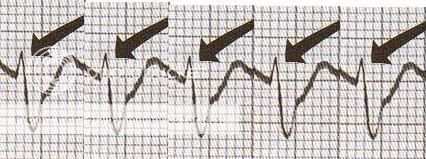
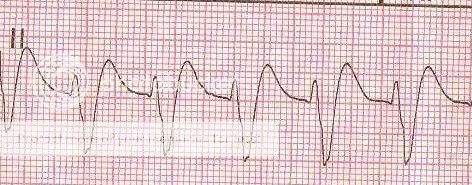
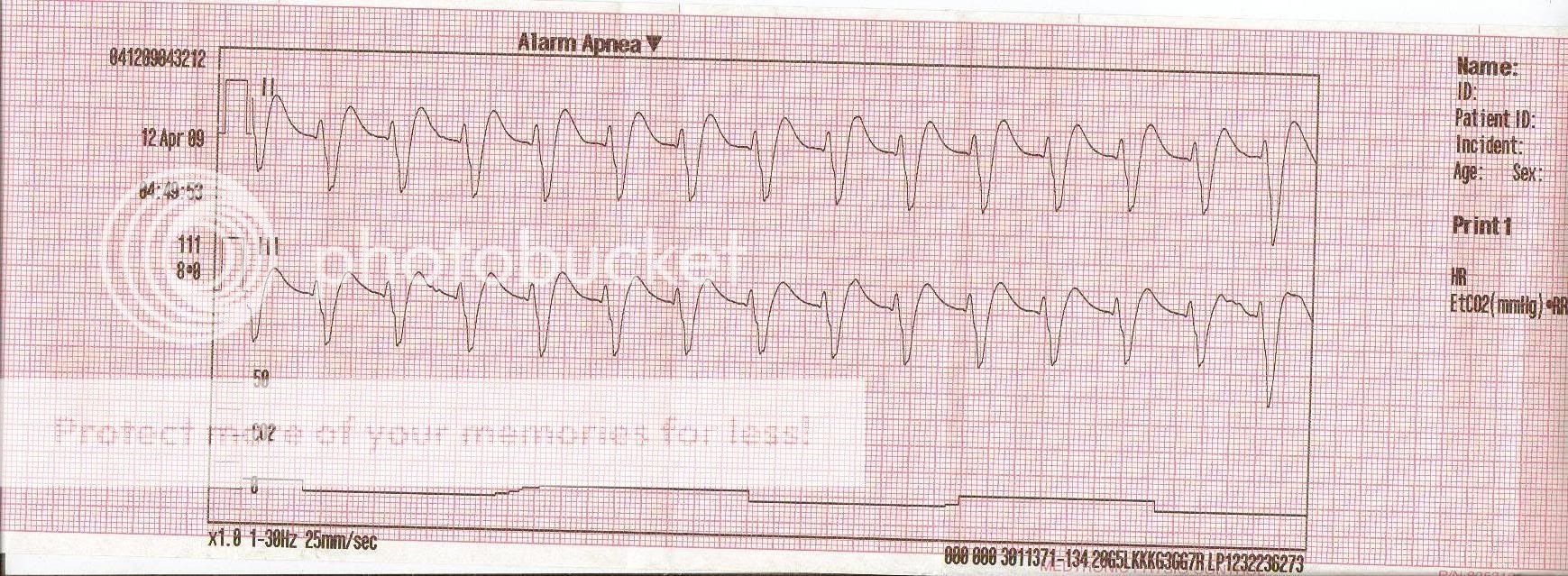
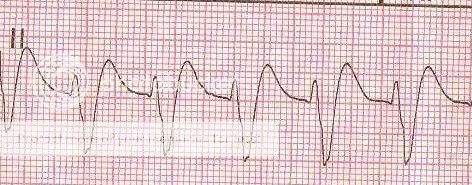
Negative on a 12-lead, as you can see other things were going down. Regardless, some sort of aberrancy?
-rye
Follow along with the video below to see how to install our site as a web app on your home screen.
Note: This feature may not be available in some browsers.
Sorry Delta I don't follow the "axis determining treatment option" remark.
I can't see such a wide rhythm originating around the AV node to make junctional a differential interpretation.
As for treatment unless your guidelines are substantially different from mine whether arrested or with a pulse even as a PEA (perhaps especially as a PEA) the pt would get electricity +/- Ventricular anti-arrhythmic and general perfusion management.
Interesting. Do you happen to have any links to any research that proves that shocking PEA is in of any benefit? Unless, by elecricity, you mean TCP for the brady PEA.
The way I see it, with PEA, there is usually an organized electrical pattern on the monitor, just without a palpable pulse. It could technically be any rhythm, although the common ones are slow and wide. So what is there to defibrillate? The cardiac cells can still be depolarizing in synch, just without either an associated physical contraction of the myocardium, or insufficient cardiac output to cause a viable pressure. Over here, PEA is all about H's, T's, Epi, and Atropine (if it is brady). More or less treated like asystole with some critical thinking thrown in.
Please note I said +/- electricity/antiarrhythmic and perfusion management. Our guidelines are the same by the sound of it.
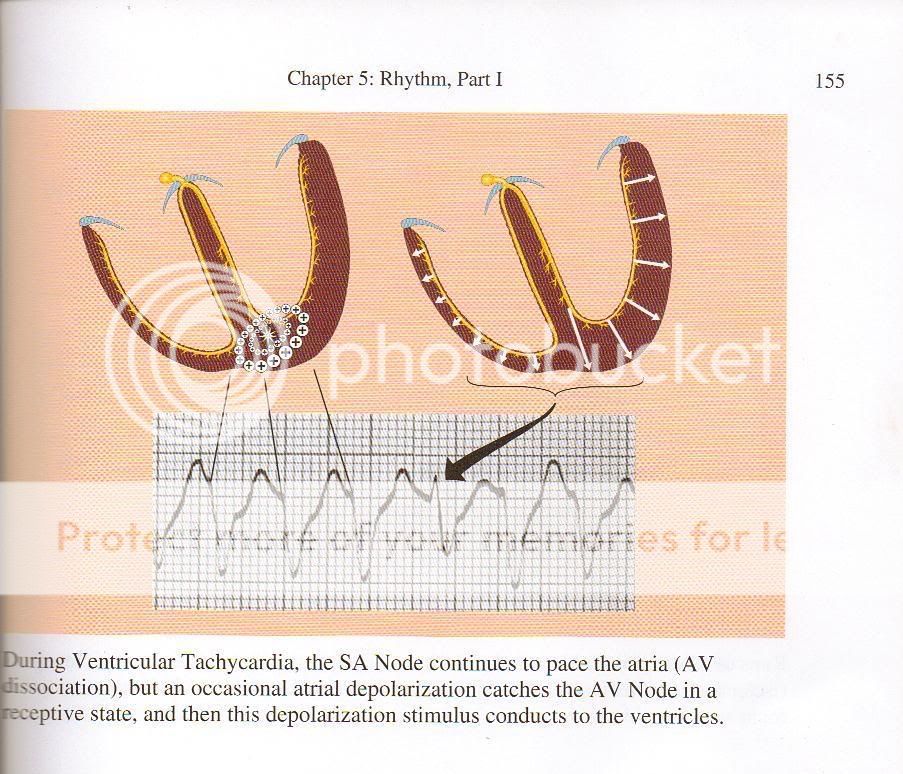
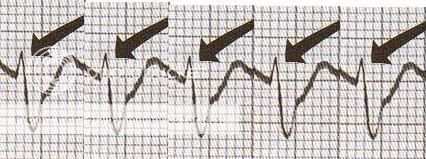
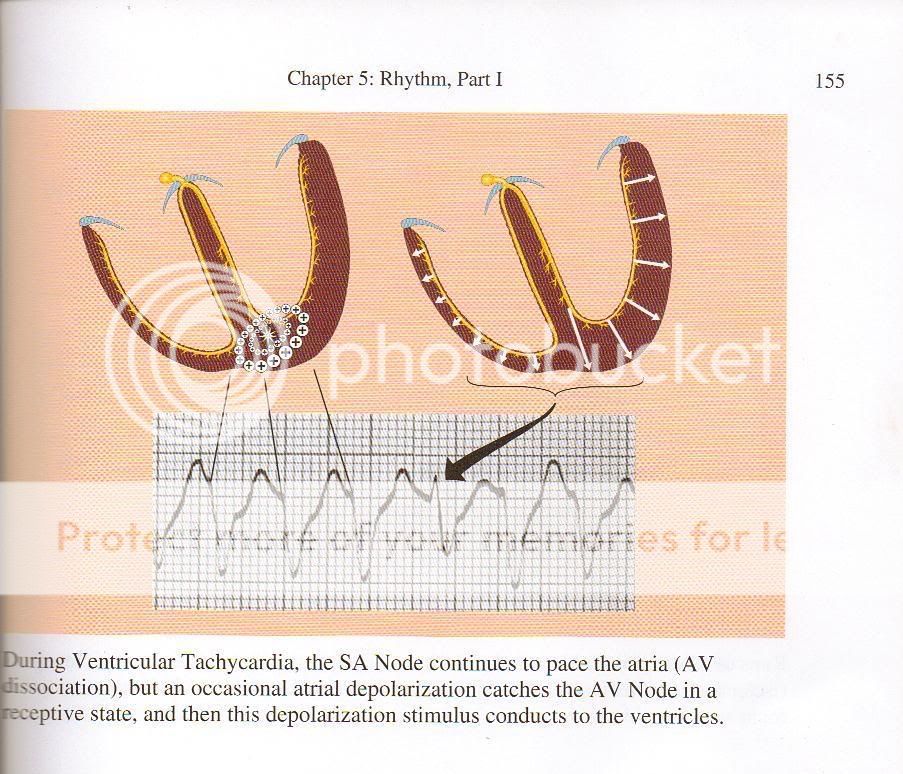
At the risk of some sort of copyright infringement (all credit to Dr. Dubin), but I came across some information while reading...