Are you sure you didn't swap the leg leads? I did that once on a medic clinical and it looked just like accelerated junctional...
It doesn't look like lead reversal to me.
If you swap the leg leads with each other then there should be no difference in the 12-lead. Two reasons. The green right leg lead is a ground lead (RL/G). Because it is not recording an electrical activity to be shown on the 12-lead, you can put it anywhere on the body and it'll still work. The other thing is that the left and right leg are considered electrically equal. If you put the red left leg (LL) lead on the right leg instead, the 12-lead still won't change.

Me demonstrating to a paramedic intern how RL/G can be put anywhere (I am not a preceptor).
If the white right arm (RA) and RL/G were swapped, Einthoven's triangle will collapse making the difference between the RA to red left leg (LL) zero since the two legs are considered to be equal. Lead II uses the RA lead (negative) to LL lead (positive). This means lead II would be near isoelectric and look almost like asystole. When I tested this on myself, all of the leads were small; I didn't think too much about it, but I suspect because the triangle becomes a line and my mean QRS vector was probably perpendicular to that line making the negative and positive side of that line about equal making everything small.
If LA is switched with RL/G, Einthoven's triangle will collapse making the difference between LA and LL to be zero for the same reason as mentioned earlier. Lead III uses LA (negative) to LL (positive) so lead III would be near isoelectric looking like asystole.
Switching the LA and RA lead just inverts the triangle. If the person would normally have normal axis, this would cause right axis deviation instead. This would be easy to spot with a negative QRS complex in lead I. I tell people that this is my #1 cause of "extreme" right axis deviation. I don't mean actually extreme right axis deviation where lead I and aVF are both negative, but that the right axis deviation is more rightward than what I would normally see with right axis deviation. The right ventricle is very small. Things that cause rightward axis is the leg leads being placed on the torso, respiratory disease (right ventricle gets larger), right ventriculcar hypertrophy, lateral wall MI, and we all know about left posterior fascicular blocks (LPFB) which is
very rare by itself; It usually presents a bifascicular block with a right bundle branch block. For most of these (excluding LPFB), the rightward axis is usually very minimal and near +90 degree still because the right ventricle is small. So if the rightward axis is more than +110-120 degree, my first thought is LA and RA lead reversal. In addition, negative P-waves being present in frontal leads that would normally have positives leads, but the P-waves are normal in the precordial lead with normal PRi (biphasic in lead V1 particularly), this would strongly support RA and LA lead reversal.
The same with switching the LL lead with any of the leads (excluding RL/G), it would just invert the triangle in another direction without it collapsing. If LL was switched with LA, lead II would look like what lead I would look like if the 12-lead was done normally. Lead I would look like what lead III would look like if the 12-lead was done normally. Lead II would look like an inverted lead III, so that would be
very close looking to lead aVL, but the positive lead would be pointing more superior or upward than a normal lead aVL. If the LL lead was switched with RA, lead III would look like a reverse lead I. Lead II would look inverted (similar to aVR, but more upward). Lead I would look like a reverse lead III similar to lead aVL, but more upward.
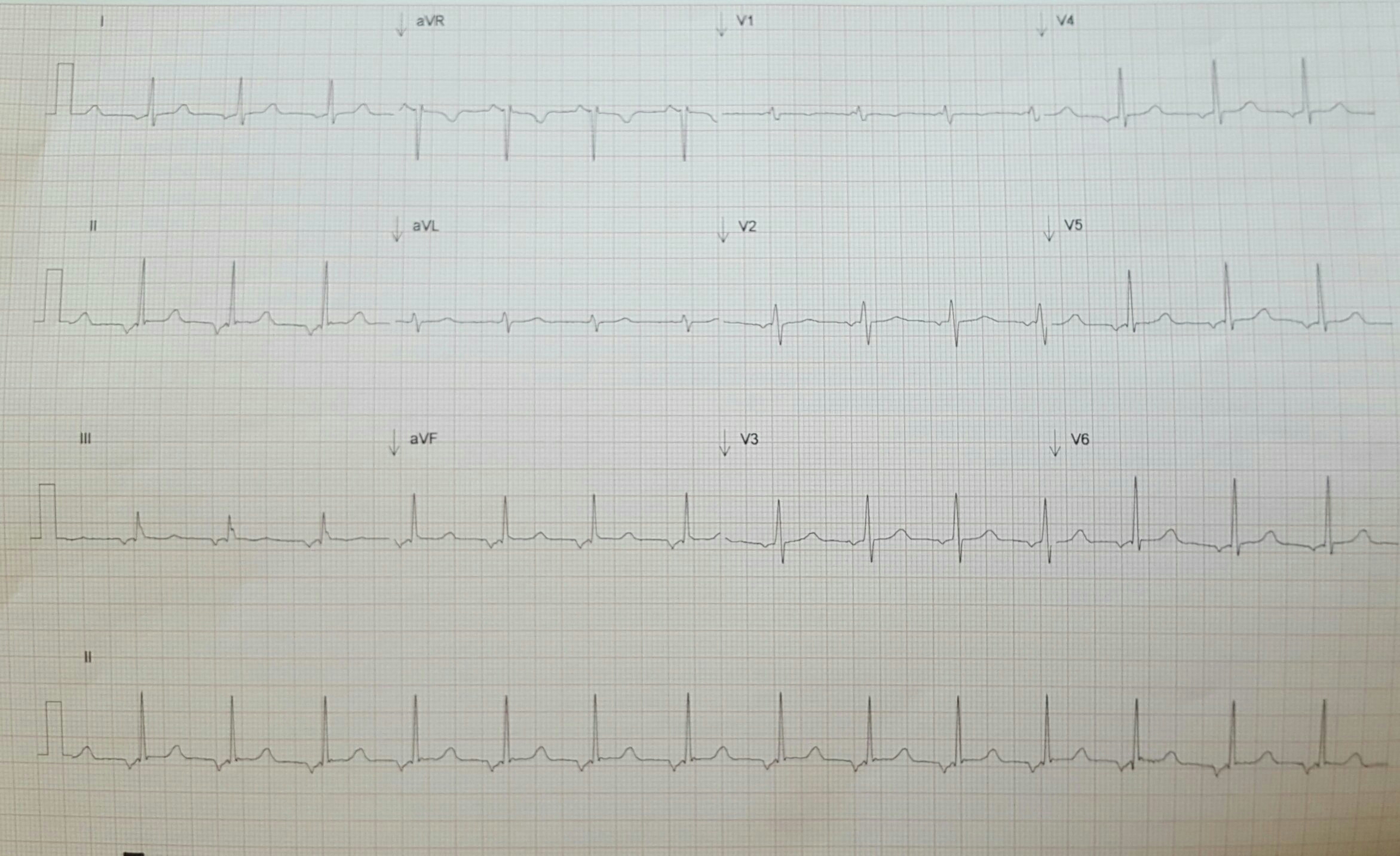
In this particular case, there is no near isoelectrical asystole looking lead in the frontal lead. This would make me not suspect reversal of the RL/G with something else. The mean QRS vector is normal looking (positive lead I and aVF, lead aVF is the smallest/closest to isoelectric making it about +60 degrees, totally normal in somebody I would suspect is slender). The leads could've been swapped making an abnormal axis look normal, but I doubt it. I do not suspect lead reversal looking at this 12-lead.
Pretty gnarly that she has inverted P-waves with a slightly shortened PRi (around 0.12s, lead V5-6 looks like the longest PRi to me). Like others mentioned, I would consider a low atrial or junctional foci.
For the same reason I explained earlier about mean QRS vector, the mean QRS vector on the transverse axis is near perpendicular to lead V1. Normally is perpendicular to lead V3-4 (around +20 to +40 degrees). In her case, it is perpendicular earlier (clockwise rotation or moved more anterolateral) at about -20 degrees instead.
I agree with the accelerated junctional, I'm just trying to put the pieces together as to why this would be existing on what should be a young and healthy heart.
The part that confuses me a bit is the low voltage in V1 and the RSr' in III (but nowhere else)
I would say lead III shows something like a qRr' (there is no downward inflection that would make it any sort of s wave). There is a small benign q-wave at the beginning of it. I would consider the finding in lead III to be non specific. It is not long enough to be considered a bundle branch block. It is still within normal limits. Probably the easiest explanation of it is that people think of the heart depolarizing as a single vector usually, but there is actually multiple vectors hence why I say mean QRS vector. Some hide or show these vectors better. That's why in a LBBB, you see the delayed depolarization of the left ventricle (second QRS) better in the lateral leads (I and V6) and delayed depolarization right ventricle in the lead positioned to the right the most (V1) in RBBB. Ironically, this terminal r' wave is something I commonly see in RBBB (I'll attach an ECG example to this).

31 year old male, flu-like symptoms, history of Tetralogy of Fallot (but this odd looking terminal deflection I've seen in many RBBB like I said).
I'm not sure why she has a low atrial or junctional rhythm. Not quite a tachycardia (I estimate the rate to be around 88 to 94). Since the rate is kinda fast for junctional the PRi is almost normal, I am thinking maybe the foci originates the atria, but not sure how sane this thought process is. Normally I think of digoxin with junctional rhythms too, which I highly doubt is the case here. I am thinking something similar to the reason why we'd see isorrhythmic AV dissociation in young people (I believe that is caused the junctional part of the heart being faster than the sinus/atria causing this benign AV dissociation with 1:1 P:QRS ratio). Instead of AV dissociation like in isorrhythmic AV dissociation, maybe her junctional is just straight depolarizing everything. I don't know. I hate coming up with crazy explanations for things....
I haven't done a lot of 12-leads on young people. On myself, I noticed that my P-waves were very hard and sometimes impossible to see. I tried a Lewis lead configuration to hide the QRS and amplify the P-wave, but it didn't work. I tried rearranging the leads solely based on my mean QRS vector and moved the leads closer to the heart similar to the the Lewis lead configuration so maybe call it pseudo Lewis, but it didn't work to hide the QRS or amplify atrial activity, lol, so not everything worked like I expected it to. I was pretty disappointed that I couldn't intentionally hide the QRS and amplify the P-wave. I wonder if it is more normal for younger people to have an atrial or junctional rhythm. Definitely see respiratory sinus arrhythmia more in young people too (including myself).
http://sixlettervariable.blogspot.com/2011/02/highlighting-atrial-activity-on-ecg-s5.html
^Written by
@Christopher from
www.ems12lead.com.
Cool ECG. Thanks for sharing.