squirrel15
Forum Captain
- 299
- 144
- 43
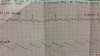
I'm an EMT-B that just started working on CCT unit, and want to learn how to read EKG's so I have a better understanding what is actually happening when I'm in the back of the rig. We mostly use 3 leads and occasionally 12 leads. Unfortunately the nurse I'm with isn't much of the teaching type. She gave me an old strip and told me to figure out what's wrong with it over the weekend. Only info I have is it was on a three lead.
At first look I was thinking afib, but considering afib is an irregular heartbeat, could this just be artifact? Because to me, it seems like the actual heartbeat is regular, since the qrs waves are spaced apart quite evenly, there is just no p or t wave.
Thanks for the help!
At first look I was thinking afib, but considering afib is an irregular heartbeat, could this just be artifact? Because to me, it seems like the actual heartbeat is regular, since the qrs waves are spaced apart quite evenly, there is just no p or t wave.
Thanks for the help!