Dispatched to memory care facility this morning for an 80's year old female complaining of abdominal pain, not alert. Patient was sitting up in a chair upon arrival with slurred speech (normal per staff). Staff states only history is hypertension. Patient was having abdominal pain and staff brought her to the restroom. Patient did not have a bowel movement. Patient brought back out to the lobby where she continued to have abdominal pain. Staff stated they obtained a radial pulse of 36 "4" times. In the ambulance abdomen palpated, no pain or guarding, no masses, however slightly distended. Vitals obtained. 166/90 pulse 60 spo2 88 on room air. O2 brought spo2 up to 96%. EKG performed (see attached). We did not have a medic at this time, this was the rhythm strip I obtained. Upon seeing that I requested a medic. 12 lead performed prior to medics arrival to have ready (Sorry, couldn't get a copy). 12 lead stated complete heart block, however the medic could not see it. Medics opinion was just sinus bradycardia. IV estabished TKO. Patients BP declined to 99/66 in short, 15 minute transport to the hospital. Any ideas on what this could have been?
Navigation
Install the app
How to install the app on iOS
Follow along with the video below to see how to install our site as a web app on your home screen.
Note: This feature may not be available in some browsers.
More options
Style variation
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
EKG Question From a Paramedic Student
- Thread starter mfd229
- Start date
FiremanMike
Just a dude
- 1,239
- 788
- 113
Hard to say without more leads, I don't see any p waves in that, but chances are i could find some in at least one of the 12 leads in order to make the call on the block..
I'd be inclined to just try some atropine and forego pacing in this case due to the short transport time and relative stability of the patient. I'd be ready to pace if anything worsens, though.
I'd be inclined to just try some atropine and forego pacing in this case due to the short transport time and relative stability of the patient. I'd be ready to pace if anything worsens, though.
281mustang
Forum Lieutenant
- 230
- 12
- 18
Definitely an odd looking ekg...
I really would like to see a copy of the 12-lead, but with such a short transport time I probably would of just given o2, gotten IV access, and monitored closely while en route.
I really would like to see a copy of the 12-lead, but with such a short transport time I probably would of just given o2, gotten IV access, and monitored closely while en route.
281mustang
Forum Lieutenant
- 230
- 12
- 18
Obviously some type of block, if pt met criteria you could potentially give atropine to rule out a 3rd degree.
As a medic student you'll come to learn that we unfortunately deal with these more than the textbook rhythms you see in class.
As a medic student you'll come to learn that we unfortunately deal with these more than the textbook rhythms you see in class.
Last edited by a moderator:
blindsideflank
Forum Lieutenant
- 184
- 3
- 18
I'm wary of a lot of the comments regarding "I wouldn't treat because of the short transport time" That is an interesting statement that opens up a whole new discussion.
Anyways, I see a complete heart block and wouldn't bother with atropine if I felt the need to treat.
Also, who took your pressures? The machine?
Anyways, I see a complete heart block and wouldn't bother with atropine if I felt the need to treat.
Also, who took your pressures? The machine?
- 5,022
- 1,422
- 113
Look at leads V1-4. Unless I'm not seeing things right, there be P waves without QRS complexes there... The 3 lead strip has no P waves at all and the QRS complexes are irregular. Could be A-Fib or really could be a complete heart block. I'm leaning toward the latter.Obviously some type of block, if pt met criteria you could potentially give atropine to rule out a 3rd degree.
As a medic student you'll come to learn that we unfortunately deal with these more than the textbook rhythms you see in class.
- 2,735
- 1,272
- 113
^Yep. Regular p-waves visible in V1-V4 without QRS. Slow and wide complex to boot? 3rd Degree Block.
Angel
Paramedic
- 1,201
- 307
- 83
Obviously some type of block, if pt met criteria you could potentially give atropine to rule out a 3rd degree.
As a medic student you'll come to learn that we unfortunately deal with these more than the textbook rhythms you see in class.
right? some stuff makes me scratch my head and i feel 'dumb' for not knowing it, but second opinions are always welcome, especially on obscure cases.
I'm wary of a lot of the comments regarding "I wouldn't treat because of the short transport time" That is an interesting statement that opens up a whole new discussion.
Anyways, I see a complete heart block and wouldn't bother with atropine if I felt the need to treat.
Also, who took your pressures? The machine?
not sure if your protocols are different, but for us atropine is contraindicated for high degree blocks (an acute MI), so if the patient was 'symptomatic' wed go straight to pacing as well.
what i find interesting is how important it is to get multiple views, because lead 3 (on lp15 our default is 2 and 3) you cant see much.
Last edited by a moderator:
blindsideflank
Forum Lieutenant
- 184
- 3
- 18
You ever use Lewis leads/S5?
And we are fortunate that we don't have protocols but pacing is the go to for me in this rhythm
And we are fortunate that we don't have protocols but pacing is the go to for me in this rhythm
You ever use Lewis leads/S5?
And we are fortunate that we don't have protocols but pacing is the go to for me in this rhythm
We don't. Not sure what those are.
Angel
Paramedic
- 1,201
- 307
- 83
i havent heard of it either but this is what i found. (i know not a super reputable source but here it is)
http://en.wikipedia.org/wiki/Lewis_lead
and

http://en.wikipedia.org/wiki/Lewis_lead
and
Last edited by a moderator:
- 5,022
- 1,422
- 113
I learned of the Lewis Lead many years ago... and that setup pretty much right, for use with standard 3 lead monitors. Another setup that is used is this:
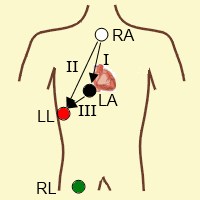
This lead is very good at seeing atrial activity. If it's present in the Lewis Lead, it will be very, very prominent. I first learned about this lead back in Paramedic School. For various reasons, I like MCL1 for monitoring, but that lead won't show P waves anywhere near as prominently as the Lewis Lead does.
In short, if you need to see if there are P waves, think Lewis Lead!
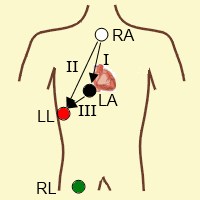
This lead is very good at seeing atrial activity. If it's present in the Lewis Lead, it will be very, very prominent. I first learned about this lead back in Paramedic School. For various reasons, I like MCL1 for monitoring, but that lead won't show P waves anywhere near as prominently as the Lewis Lead does.
In short, if you need to see if there are P waves, think Lewis Lead!
Bearamedic
Forum Crew Member
- 42
- 0
- 6
Things i see:
the axis deviation, the pwaves without qrs, the qrs without a p wave, the slightly wide qrs, deep swave in III, the avl positive vs the avf negative deflections.
My conclusion:
3rd degree (junctional escape focus) and left anterior fasicular block
I would have liked to have more complexes though.
the axis deviation, the pwaves without qrs, the qrs without a p wave, the slightly wide qrs, deep swave in III, the avl positive vs the avf negative deflections.
My conclusion:
3rd degree (junctional escape focus) and left anterior fasicular block
I would have liked to have more complexes though.
Christopher
Forum Deputy Chief
- 1,344
- 74
- 48
Any ideas on what this could have been?
Between the 3-Lead and 12-Lead it appears that there is a high degree AV block present, but not necessarily complete. The variable R-R intervals on the 3-Lead shows that occasional capture is present. The P-P intervals are roughly 50 bpm, so we'll go with:
Sinus bradycardia, high degree AV-Block, with an escape perhaps out of the right bundle branch? Quite the slow V-rate.
Christopher
Forum Deputy Chief
- 1,344
- 74
- 48
Based on the EKG, would that warrant transport to a cardiac specialty hospital or is any hospital capable of treating heart blocks?
It depends on your area hospitals' setup. I wouldn't take the patient to a community hospital for certain
It would make sense that any hospital with an emergent cath lab could handle this patient as they would likely do pacemakers as well...but you never know!
- 4,533
- 3,258
- 113
Pretty much anyplace can float a temporary pacer.....but I would agree that a patient like this should go to a cardiac specialty center, if the difference in transport time isn't too long. That type of thing would ideally be addressed in your destination protocols.
NPO
Forum Deputy Chief
- 1,831
- 897
- 113
Took a manual BP the first time, confirmed it with the monitor. From there on pressures came off the monitor.
To me that's backwards. I'll do an automated one and a manual to confirm the machine. I don't trust them.

