Smellypaddler
Forum Probie
- 27
- 4
- 3
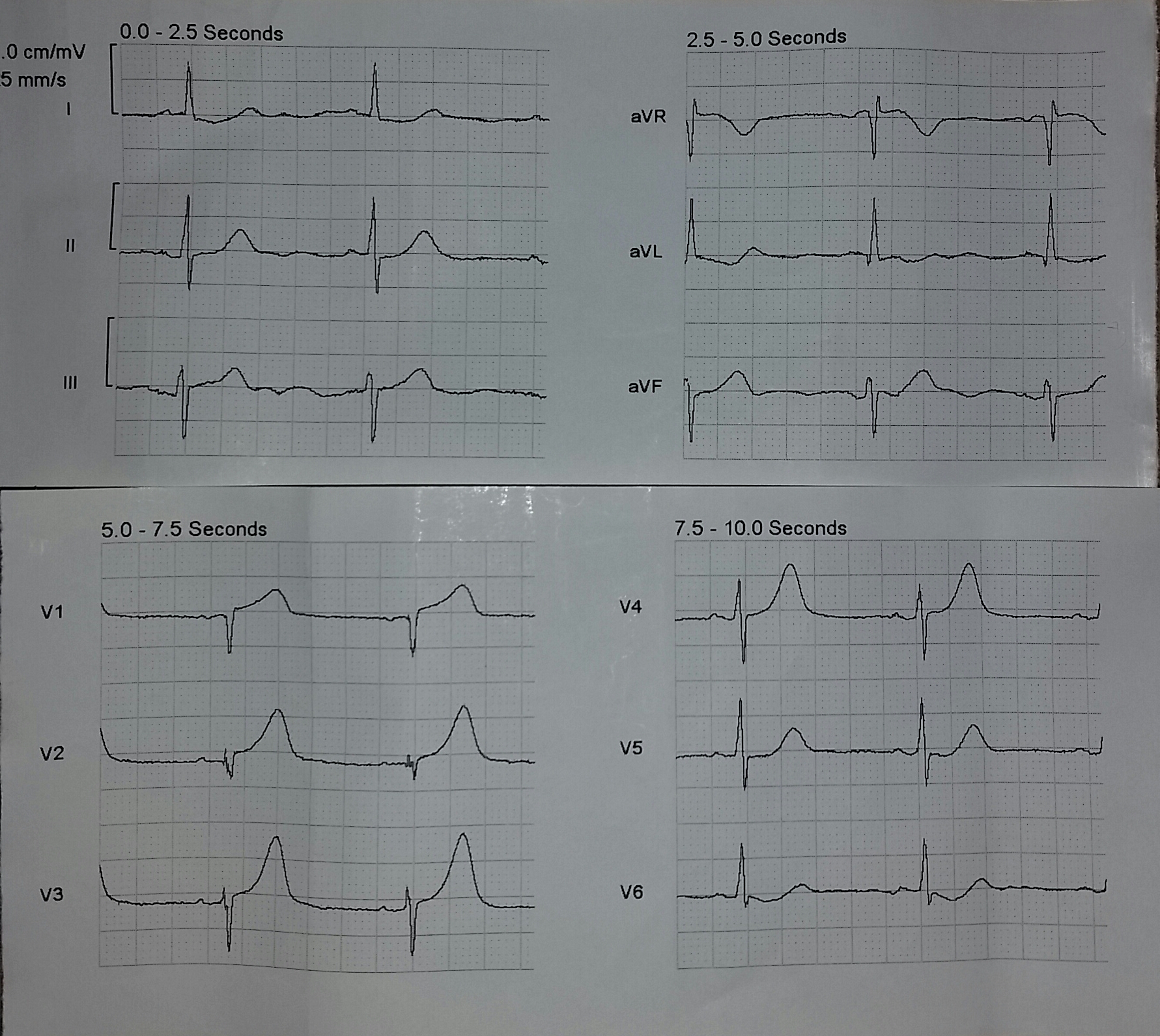
70yoF who presented with 9/10 central chest pain, associated diaphoresis and vomiting.
Pain described as stabbing in nature, worse on inspiration and palpation.
The Zoll auto-diagnosis only states "moderate ST depression" no finding of infarction.
I'm just wondering what others would think of this ECG and how they would treat based on the ECG and presenting symptoms?
No other tricks or funny business: Nil Phx, Nil meds, normally fit and well, NKDA.
Vitals stable:
BP= 140/systolic
RR = 16
Afebrile
Pain described as stabbing in nature, worse on inspiration and palpation.
The Zoll auto-diagnosis only states "moderate ST depression" no finding of infarction.
I'm just wondering what others would think of this ECG and how they would treat based on the ECG and presenting symptoms?
No other tricks or funny business: Nil Phx, Nil meds, normally fit and well, NKDA.
Vitals stable:
BP= 140/systolic
RR = 16
Afebrile
