Christopher
Forum Deputy Chief
- 1,344
- 74
- 48
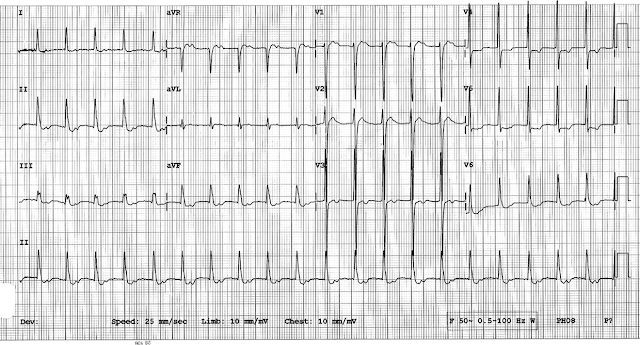
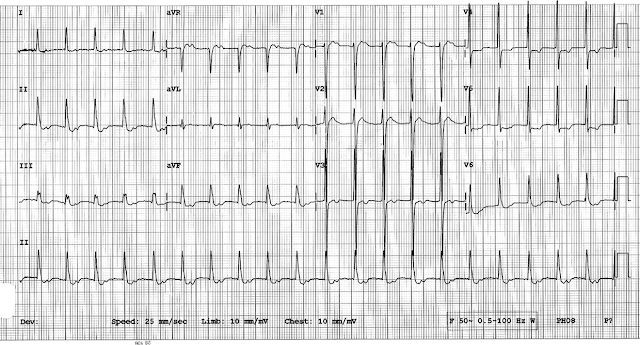
(These ECG's are from a paper I was reading and represent a good interpretation and diagnosis to have locked away in your memory)
66 year old female, ECG #1 from the outlying hospital. ECG #2 is from after transfer at a larger academic hospital.
No history, no nothing, because everybody loves a cold read!

66 year old female, ECG #1 from the outlying hospital. ECG #2 is from after transfer at a larger academic hospital.
No history, no nothing, because everybody loves a cold read!