Usually arrhythmias have a blanket treatment depending on whether the patient is symptomatic due to the rate being too fast or slow. You'd follow the ACLS algorithm for symptomatic bradycardia or tachycardia. Common drugs for bradycardia are atropine, dopamine, and epinephrine. Common drugs for tachycardia are adenonsine, lidocaine, and amiodarone. Unstable patients are treated with electricity.
Some rhythms can have specific treatment. For example, atrial fibrillation and atrial flutter can be treated with calcium channel blockers such as diltiazem and verapamil. Fascicular VT may also be treated with calcium channel blockers.
It's not usually recommended to treat PVCs. They are very commonly ignored. Where I did my paramedic internship at, paramedics were allowed to treat frequent PVCs with lidocaine, but not anymore. I believe these patients used to be treated with class Ic antiarrhythmics, but that was discontinued.
From what I've learned, 2nd degree AVB type I (Wenckebach) is usually tolerable and does not require treatment. I've only appreciated this or recognized this once in a patient that was being discharged from the hospital after being treated for pneumonia.
I've heard that 2nd degree AVB type II (Mobitz), 3rd degree AVB, or patients with heart transplant do not respond to atropine.
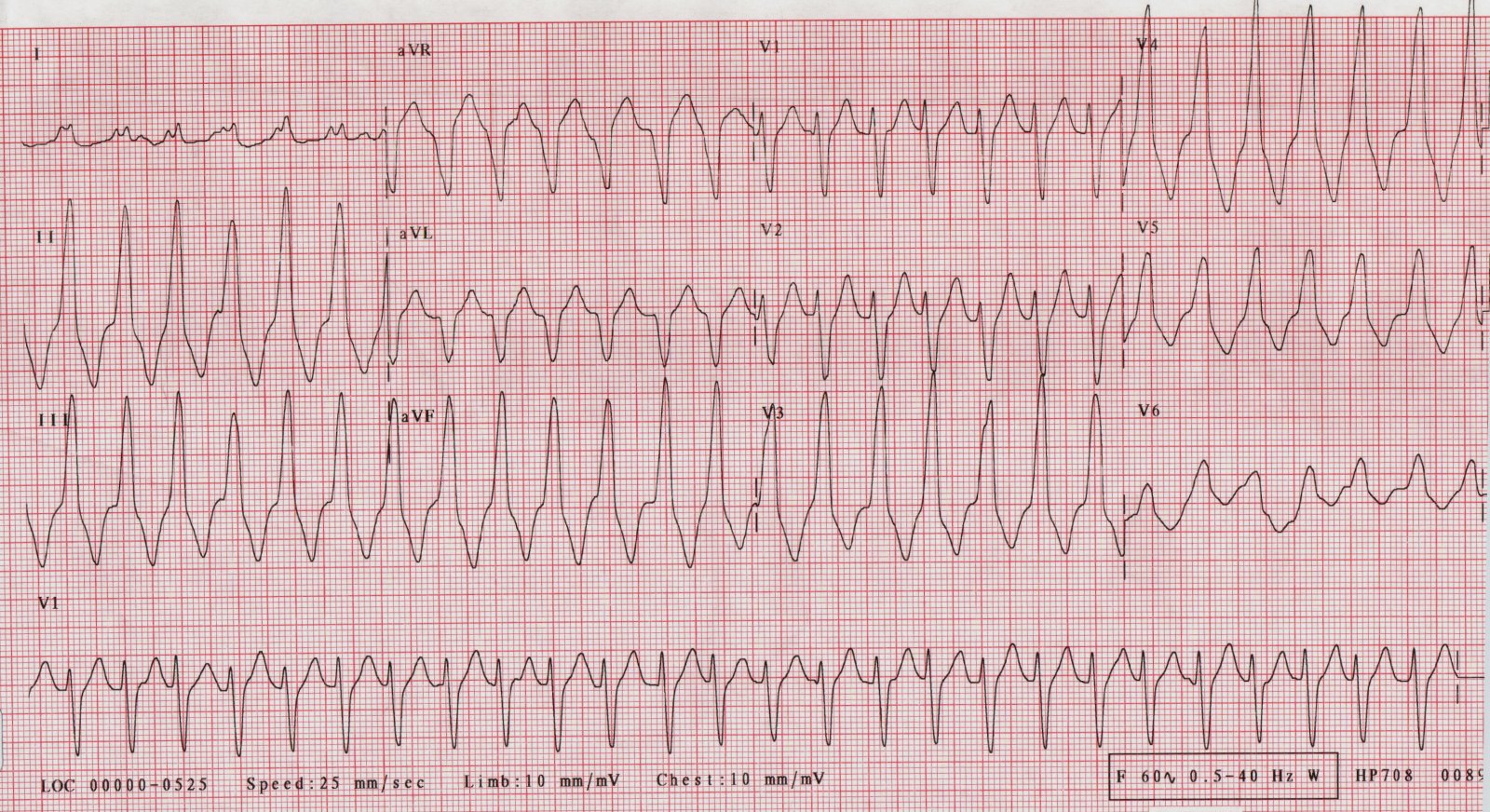
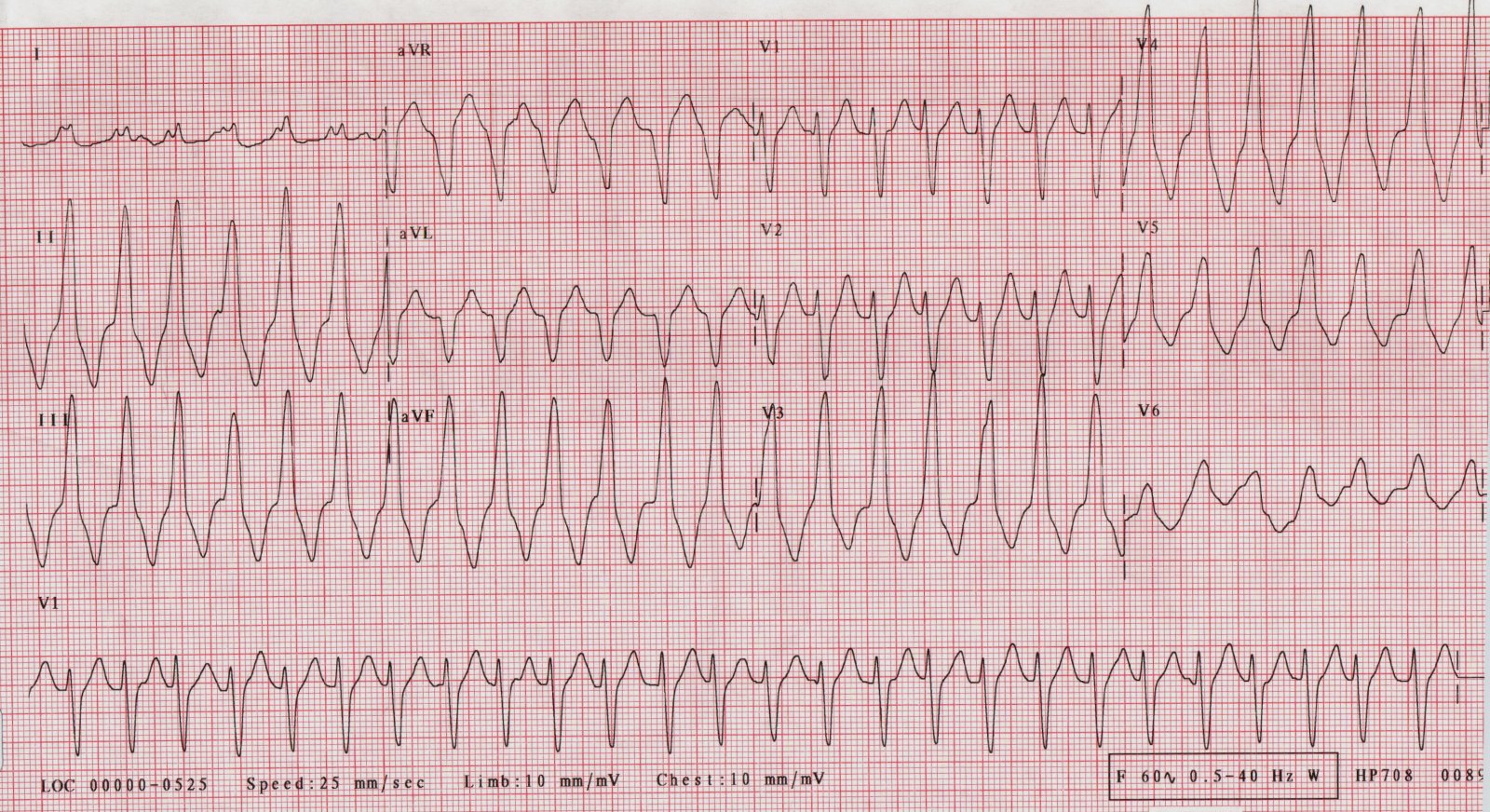
There are many criteria used to differentiate VT vs SVT with aberrancy. The most common one I've seen used or discussed is Brugada's criteria.
Step 1 Are there any RS complexes in the precordial leads (leads V1-V6)? If not, it's VT.
Another way people may ask this is are the precordial leads all concordant ie are they all positive or all negative. If they are, it's VT.
If VT is not diagnosed, move to step 2.
Step 2 In any of the precordial leads with an RS wave, is the R-wave wide? Specifically is from the start of the R-wave to the nadir of the S-wave (pointy tip of it) at least 100 ms? If so, it's VT.
This step alone is called Brugada's sign. I'm not sure if the sign can be used in any lead. I've never read anything that has specified it. In Brugada's criteria or algorithm for VT, it is only the precordial leads.
If VT is not diagnosed, move to step 3.
Step 3 Is there AV dissociation? Do the P-waves not correlate with the QRS complex? If so, it's VT.
In my opinion, this is one of the worst criteria. It's usually hard to differentiate this from artifact. Try to march out the P-waves if you think you see it. I usually skip this step.
If VT is not diagnosed, move to step 4.
Step 4 Does it have typical bundle branch block (BBB) morphology? If not, it's VT.
Some people ask instead if it has typical VT morphology instead. I do not like this way. If it does have typical VT morphology, it's VT.
If neither meet VT criteria in step 4 and you've gone through all the step, that favors SVT with aberrancy.
BBB Morphology
BBB morphology is usually the first thing I notice when differentiating VT vs SVT with aberrancy. It's usually the quickest and easiest way for me to recognize it is VT.
I look at lead V1 first to determine if it is closest to right BBB (RBBB) morphology or left BBB (LBBB) morphology. If V1 is positive, I'll look for RBBB morphology. If V1 is negative, I'll look for LBBB morphology.
Typical morphology for RBBB in lead V1 is an rsR' wave. It can have a qR wave, but I've read this is more favorable for VT if it has this instead.
Typical morphology for LBBB in lead V1 is an rS wave and the R-wave is very very very small and narrow.
I'll then look at lead I and V6.
In RBBB, lead I and V6 will have an Rs wave ("slurred S wave").
In LBBB, lead I and V6 will have a mostly (if not all) positive R-wave. Sometimes the R-wave will have a little dip in the center of it, but nothing that comes even close to the isoelectric line.
It is commonly taught that 0.12s or greater is used to diagnosed bundle branch block. This I think is taught for simplicity and ease. The right side of the heart (pumping only to the lungs) is way smaller than the left side of the heart (pumping to the rest of the body). If the right side of the heart is last depolarize (like in RBBB), it is usually takes less time for the right side depolarize versus the left side of the heart because there is less tissue. So I believe some people teach that RBBB can be diagnosed even the width of the QRS complex is 0.11s (because the right side is smaller). I have not commonly seen or heard of this though. This does apply to one thing in regard to interpreting VT. If it is RBBB-like morphology and the QRS >0.14s, it favors VT. If it is LBBB-like morphology and the QRS >0.16s, it favors VT. Very wide complexes are very favorable for VT, but can also be due to metabolic disorders (hyperkalemia) or drug overdose (sodium channel blocker).
With practice, you can immediately recognize it is very likely it is VT at just a glance.
The reason I kind of like this criteria the most is interesting, but I am not sure if it is correct. I'll explain it anyhow. The foci of the VT changes the morphology of the QRS complex. If the foci originates from the right ventricle, it'll have LBBB-like morphology. If the foci originates from the left ventricle, it'll have RBBB-like morphology. I believe this is for the same reason you see LBBB and RBBB. In LBBB, the left side of the heart is last to depolarize because of a block on the left side. In RBBB, the right side of the heart is last to depolarize because of a block on the right side. It makes sense that if the foci is on the right side, the right side depolarize first and the left side is last to depolarizing giving it LBBB-like morphology. It makes sense that if the foci is on the left side, the left side is depolarizing first and the right side is last to depolarize giving it a RBBB-like morphology. This also means that where the foci is, the QRS morphology is going to change. The QRS morphology says a lot about where the foci originates. This is true for paced rhythms also (where the pacer wires are placed). Anyhow, since the foci can be anywhere in the ventricles in VT, the QRS morphology can vary a lot with VT! However, SVT stands for supraventricular tachycardia. Surpa means above. Supraventricular means above the ventricle. This means that the ventricles are almost always depolarized starting at the top from the AV node (unless there is an accessory pathway like with Wolff Parkinson White syndrome, which can be indistinguishable from VT if the rhythm is an antidromic AVRT) and down. This means SVT with aberrancy will usually have a very predictable QRS pattern while VT will not. This also means that there are a lot of criteria that are very specific to VT (ie if the finding is present, it is very likely to be VT because SVT is unlikely to make that finding), but is not sensitive (ie just because the finding is not present doesn't mean it is not VT... because VT can present in all shapes and forms depending on the foci). Hope that makes sense!
Other criteria people use is looking for extreme right axis deviation. That is lead I is negative, lead aVF is negative, and lead aVR is positive. This is pointing up and to the right of the heart (left from our point of view). This is for the same reason that the foci originating from the left side of the heart makes RBBB-like morphology and foci originating from the right side of the heart makes LBBB-like morphology. If the foci originates from the bottom of the heart, the bottom of the heart is first to depolarize and the top part of the heart is last to depolarize making the mean QRS vector pointing up. The apex of the heart is at the left ventricle so up and to the right (extreme right axis deviation) means the foci most likely originated from the apex.
Earlier I said
This also means that there are a lot of criteria that are very specific to VT (ie if the finding is present, it is very likely to be VT because SVT is unlikely to make that finding), but is not sensitive (ie just because the finding is not present doesn't mean it is not VT... because VT can present in all shapes and forms depending on the foci).
People make the grave mistake of thinking that lack of extreme right axis deviation means that it is not VT. This is incorrect. This means that the foci probably didn't originate at the apex of the heart, but it could have still originated from the ventricles. VT can have any axis like Tom said (eg septal fascicular VT will have RBBB morphology with normal axis).
The other thing is looking for fusion or captured beats. You'll see wide complex tachycardia and then all of the sudden a lone (or couple of) narrow regularly looking beats (capture beat) and/or semi wide beats that are like an in between PVC and regular beat (fusion beat). Very specific for VT with AV dissocation where the atria and ventricle happen to depolarize at the perfect time.
As crazy as this may sound, VT can have 1:1 conduction of the atria! It'll conduct from the ventricle up into the atria creating a P-wave after the QRS complex. A P-wave being present shortly after the QRS complex does not rule out VT.
Another thing people look for is notching between beginning for the S-wave to the nadir of the S-wave called Josepheson's sign.
Older patients (>35 years old) and history of heart disease (eg MI) increase the likelihood of it being VT. Being young doesn't rule out VT.
I totally agree with "VT until proven otherwise". One of my favorite differential I've seen posted for wide complex tachycardia is
1. VT
2. VT
3. VT
4. VT
5. VT
6. VT
7. VT
8. VT
9. VT
10. SVT with aberrancy
If you are thinking it is possibly VT, it probably is VT.
This is really beyond what they usually teach at paramedic school, but I couldn't help myself typing this. This is about the only paramedic thing I am good at. :[