This more pertains to critical care paramedicine, but I was wondering: how do you remember what each vent mode (A/C PRVC SIMV etc) does when ventilating a patient? Any tricks (or charts) to remembering what each one does?
There are apps that I carry, and peruse from time to time on my phone (basics of mechanical ventilation is the one I review the most from time to time, and it has the modes you've listed in your post). Just know with ventilator management there is no one-size fits all approach.
I also recommend giving Eric Bauer's book on prehospital ventilator management a look, as well as his, and Weingart's podcasts. They have some stuff that is unconventional though, and requires quite a bit of experience (many of it far beyond even my comfort zone, and level), and may not be well received by the masses at your particular program. YouTube, and Google also did wonders---and still do---when I first began delving into vent management.
If you have any RRT/ RCP colleagues, pick their brains; if you run into any pulmonologists pick theirs as well. Understand everything there is about the respiratory system to the best of your ability from basic adjuncts (e.g., never not transport your vented patients without a BVM/ mask at the ready, and easily accessible to you), get familiar with ABG's, and different formulas that may benefit certain patient types (e.g., Winter's Formula for a critically ill intubated, and ventilated metabolically acidotic patient), and get familiar with the ARDS net group, their literature, and publications.
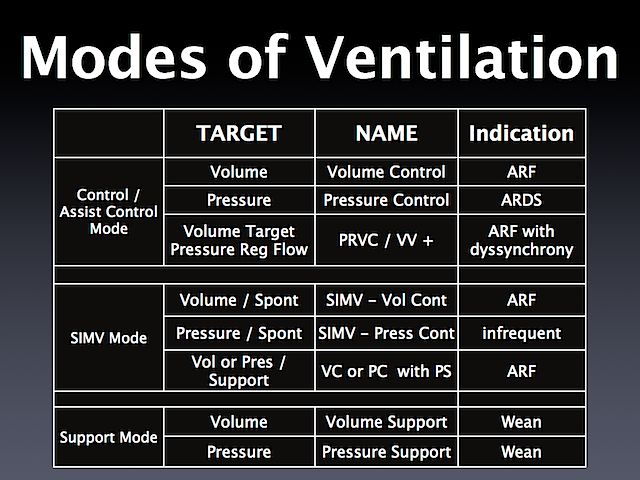
Also, consider the type of ventilator you use, and get to know it back, and forth, play with it, do routine vent checks til you're comfortable with the basic set ups and modes. As far as when to use to different modes/ what they do, again, you will hear 10 different people cite 10 different uses. If your ventilator has PRVC, then you're well ahead of most of the soon-to-be phased out prehospital vents as this is a combination mode which as the name implies offers volume-control ventilation while calculating the patients initiated pressure limits so to speak. You may also see CMV-assist listed as AC, CMV alone is a pretty obsolete mode that has very limited use at least at my program. I hope this helps you some

.