Called out for chest pain around 10pm, 50 year old female complaining of chest pain and also fell down.
Upon arrival find 50 year old female lying in floor in living room complaining of chest pain and headache and she "hit her head". Patient states she fell down and she doesn't know why, hit her head on the carpet. Patient has also been having intermittent chest pain for 3 days, a couple times a day. But about 2.5 hours ago it has become constant sharp pain 8/10, substernal on the left side extending around the ribs to her back. Patient denies neck or back pain or additional trauma.
Patient has a medical history of migraine headaches with accompanied seizures a few times a month, however states that only happens if she messes up her medications. Patient takes Tramadol, gabapentin, and amitriptyline. Patient is compliant with her meds. Patient has no other medical history at all. Patient sees primary care on a regular basis and states she has not been to a hospital at all in over 15 years. Only surgical history was a knee replacement when she was in her early 30's.
Onset of chest pain 2.5 hours ago accompanied by shortness of breath with chest pain worse upon inspiration but not palpation. Patient states no nausea. Patient is midly diaphoretic and appears not well. Patients family has history of heart problems, father, two brothers, and two uncles have all died from cardiac related problems and another uncle has had a heart transplant. Patient is in good shape, relatively athletic, smokes a few ciggarettes a day and consumes no alcohol and does no drugs. Patient is 5'9 and ways 145.
Initial vitals are
BP - 160/100
HR - 84
O2 % - 98 on room air
RR - 20 and shallow (All lung fields clear)
BgL - 98
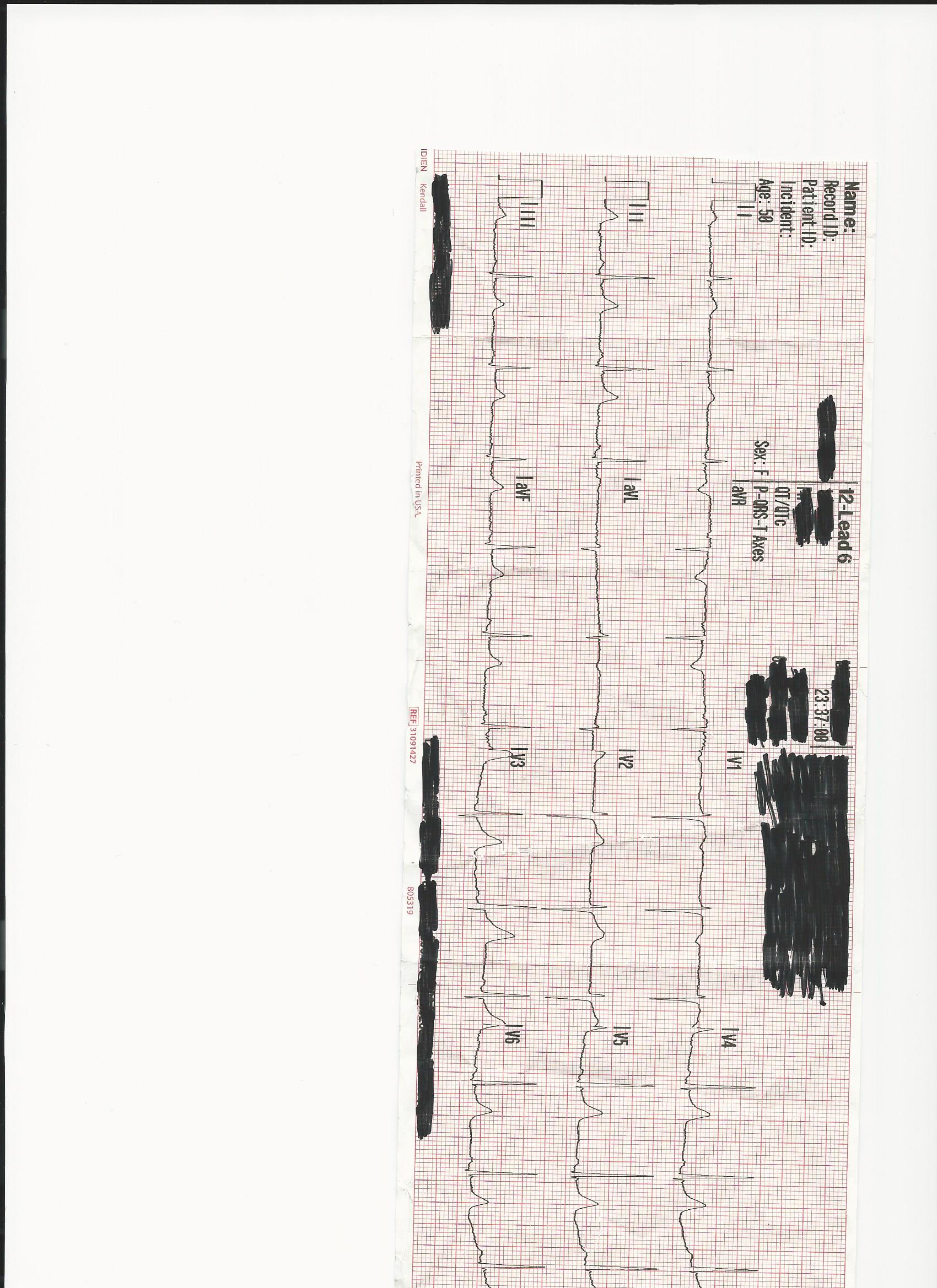
this is the third 12 lead obtained a couple minutes after getting her in ambulance, patient appears anxious, short of breath, and in substantial pain.
Any concern from the 12 lead? Community band aid station is 5 minutes priority2.... PCI center is 30 minutes priority1.... Trauma Center/PCI center is 1 hour priority1 or a hop skip and a jump by helicopter.
Course of action? Decision making process? is this a "standard" chest pain call for you?
If you have any additional questions I can likely provide answers about patient presentation.
Upon arrival find 50 year old female lying in floor in living room complaining of chest pain and headache and she "hit her head". Patient states she fell down and she doesn't know why, hit her head on the carpet. Patient has also been having intermittent chest pain for 3 days, a couple times a day. But about 2.5 hours ago it has become constant sharp pain 8/10, substernal on the left side extending around the ribs to her back. Patient denies neck or back pain or additional trauma.
Patient has a medical history of migraine headaches with accompanied seizures a few times a month, however states that only happens if she messes up her medications. Patient takes Tramadol, gabapentin, and amitriptyline. Patient is compliant with her meds. Patient has no other medical history at all. Patient sees primary care on a regular basis and states she has not been to a hospital at all in over 15 years. Only surgical history was a knee replacement when she was in her early 30's.
Onset of chest pain 2.5 hours ago accompanied by shortness of breath with chest pain worse upon inspiration but not palpation. Patient states no nausea. Patient is midly diaphoretic and appears not well. Patients family has history of heart problems, father, two brothers, and two uncles have all died from cardiac related problems and another uncle has had a heart transplant. Patient is in good shape, relatively athletic, smokes a few ciggarettes a day and consumes no alcohol and does no drugs. Patient is 5'9 and ways 145.
Initial vitals are
BP - 160/100
HR - 84
O2 % - 98 on room air
RR - 20 and shallow (All lung fields clear)
BgL - 98
this is the third 12 lead obtained a couple minutes after getting her in ambulance, patient appears anxious, short of breath, and in substantial pain.
Any concern from the 12 lead? Community band aid station is 5 minutes priority2.... PCI center is 30 minutes priority1.... Trauma Center/PCI center is 1 hour priority1 or a hop skip and a jump by helicopter.
Course of action? Decision making process? is this a "standard" chest pain call for you?
If you have any additional questions I can likely provide answers about patient presentation.
