This is one I had last week...
You are at an event working BLS without transport capability (backpack EMT), standard BLS loadout. Delay for ALS response is 25 minutes, 60 minutes for chopper. Nearest facility is 30 min. away by ground, all Las Vegas hospitals 25 - 30 minutes away by air after waiting for chopper.
Call comes in for a patient who "feels funny" and wanted to get into the AC to cool down. Outside temp is 112 F and 5% humidity.
Pt. presents with chief complaint of transient tunnel vision (which abated once removed from heat) and a flutter feeling in his chest. He is A&O x 4, calm, patent airway, breathing unlabored @ 12 rpm, radial pulse x2 @ 35 strong & regular (but extremely slow), BP 148/85, SpO2 @ 98 on room air, skin pink, cool, and dry, lungs clear and equal BILAT and pt. is neurologically intact.
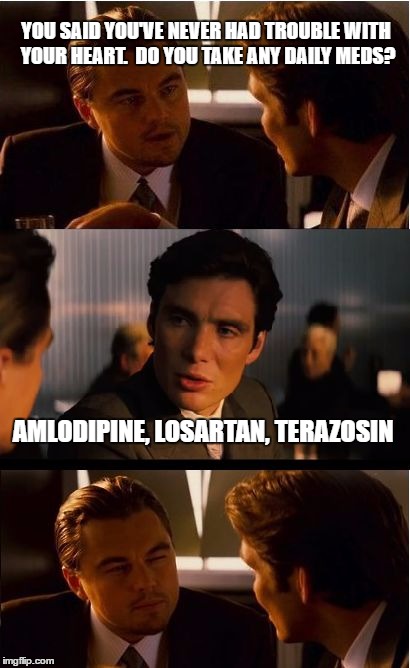
HPI - onset 15 min prior to call of "funny feeling" and partial tunnel vision. Position/activity change does not provide relief, though tunnel vision abated after removal from heat. Feeling localized to central chest without radiation or referral. Pt. denies description of "pain" and insists on calling it a "fluttery weird feeling" and once called it "slight pressure". No severity score given. Pt. reports allergy to penicillin only. Medications consist of Amlodipine, Losartan, Paroxetine, Terazosin.
PMI - pt. denies any cardiac, stroke/TIA, nor hx of respiratory problems, but admits to high cholesterol, BPH, HTN. Pt. refuses to disclose any further hx.
Approx. 5 min after initial vitals, second set taken: HR 68 RR 12 unlabored BP 140/90 SpO2 97 on room air.
ALS called due, primarily, to the brady HR, but also a "bad feeling" about this guy - response time 25 minutes. Pt. insisted he is fine, does not need an ambulance, and wants to just rest for a while before rejoining group. Pt. is told that he can refuse the ambulance when it arrives but his participation is over until cleared by Dr.
5 min. later, vitals are HR 35 RR 12 unlabored BP 148/96 SpO2 98 on room air.
Pt. is remaining absolutely calm and mentally consistent throughout.
15 min later, vitals are HR 62 RR 12 unlabored BP 146/96 SpO2 98 on room air.
What is your field assessment and what do you do for 25 minutes while waiting for ALS?
You are at an event working BLS without transport capability (backpack EMT), standard BLS loadout. Delay for ALS response is 25 minutes, 60 minutes for chopper. Nearest facility is 30 min. away by ground, all Las Vegas hospitals 25 - 30 minutes away by air after waiting for chopper.
Call comes in for a patient who "feels funny" and wanted to get into the AC to cool down. Outside temp is 112 F and 5% humidity.
Pt. presents with chief complaint of transient tunnel vision (which abated once removed from heat) and a flutter feeling in his chest. He is A&O x 4, calm, patent airway, breathing unlabored @ 12 rpm, radial pulse x2 @ 35 strong & regular (but extremely slow), BP 148/85, SpO2 @ 98 on room air, skin pink, cool, and dry, lungs clear and equal BILAT and pt. is neurologically intact.
HPI - onset 15 min prior to call of "funny feeling" and partial tunnel vision. Position/activity change does not provide relief, though tunnel vision abated after removal from heat. Feeling localized to central chest without radiation or referral. Pt. denies description of "pain" and insists on calling it a "fluttery weird feeling" and once called it "slight pressure". No severity score given. Pt. reports allergy to penicillin only. Medications consist of Amlodipine, Losartan, Paroxetine, Terazosin.
PMI - pt. denies any cardiac, stroke/TIA, nor hx of respiratory problems, but admits to high cholesterol, BPH, HTN. Pt. refuses to disclose any further hx.
Approx. 5 min after initial vitals, second set taken: HR 68 RR 12 unlabored BP 140/90 SpO2 97 on room air.
ALS called due, primarily, to the brady HR, but also a "bad feeling" about this guy - response time 25 minutes. Pt. insisted he is fine, does not need an ambulance, and wants to just rest for a while before rejoining group. Pt. is told that he can refuse the ambulance when it arrives but his participation is over until cleared by Dr.
5 min. later, vitals are HR 35 RR 12 unlabored BP 148/96 SpO2 98 on room air.
Pt. is remaining absolutely calm and mentally consistent throughout.
15 min later, vitals are HR 62 RR 12 unlabored BP 146/96 SpO2 98 on room air.
What is your field assessment and what do you do for 25 minutes while waiting for ALS?